What is Scabies?
Scabies is a highly contagious skin condition that causes severe itching, particularly at night. It occurs when tiny mites called Sarcoptes scabiei var. hominis burrow into the top layer of human skin. These microscopic parasites are specifically adapted to live on humans and cannot survive long without human contact, making person-to-person transmission the primary way the condition spreads.
The name “scabies” comes from the Latin word “scabere,” meaning “to scratch,” which perfectly describes the most troublesome symptom patients experience. This ancient condition has affected humans throughout history, but remains a significant health concern today, affecting millions of people worldwide regardless of age, race, or social status.
The Tiny Culprit: Understanding the Scabies Mite
The scabies mite is an extraordinary example of parasitic adaptation. Sarcoptes scabiei var. hominis is so small that it’s invisible to the naked eye, measuring only about 0.3-0.4 millimeters in length. The mite has a distinctive oval, flattened shape that allows it to move efficiently through the layers of human skin.
Female mites are larger than males and are responsible for the symptoms patients experience. After mating on the skin surface, the female mite uses specialized mouthparts to burrow into the outermost layer of skin, creating tunnels where she lays her eggs. This burrowing process and the mite’s waste products trigger the intense itching that characterizes scabies.
The mite’s life cycle is remarkably efficient, taking only 10-14 days from egg to adult. During her 4-6 week lifespan, a female mite can lay 2-3 eggs daily, each of which develops through several stages before becoming a mature, reproductive adult. This rapid reproduction cycle explains why scabies can spread quickly through households and communities.
How Scabies Spreads
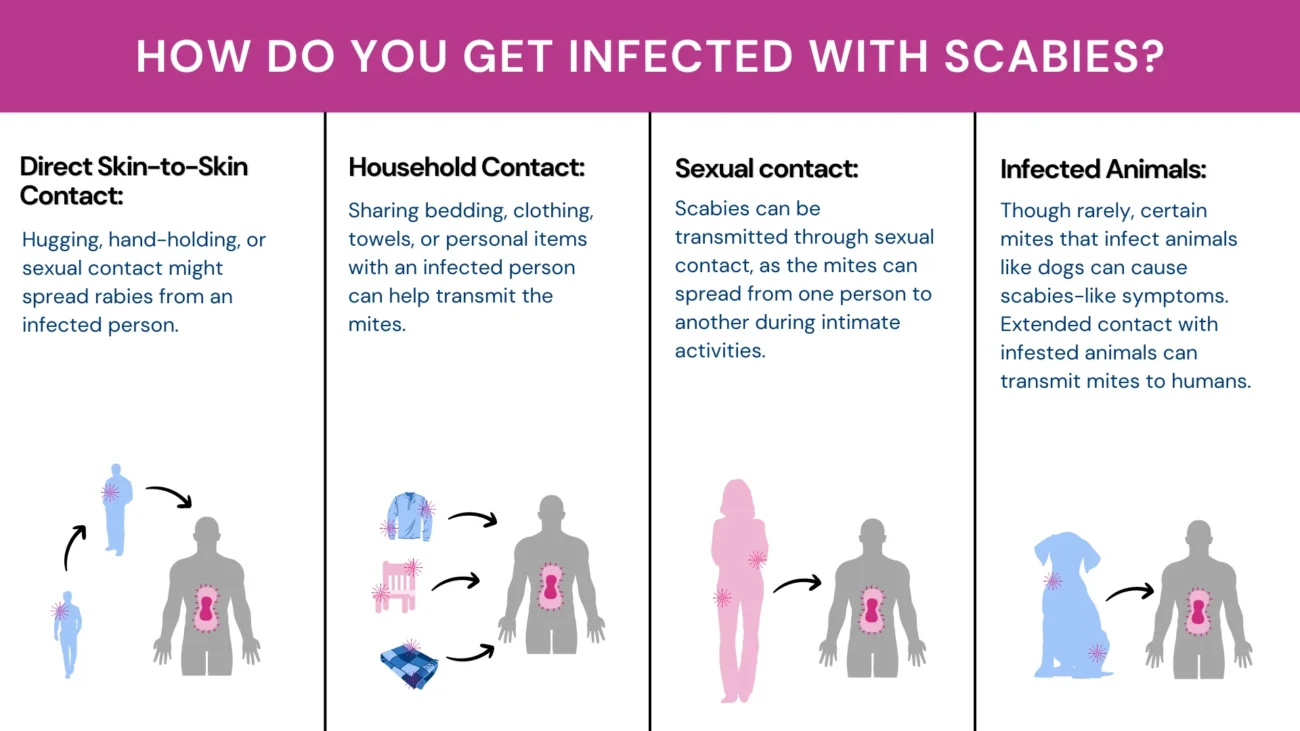
Direct Person-to-Person Contact
Scabies spreads primarily through close, prolonged skin-to-skin contact with an infected person. The mites cannot jump or fly, so they must crawl from one person to another. This typically requires at least 15-20 minutes of direct contact, which explains why scabies often spreads between:
- Family members living in the same household
- Sexual partners
- People sharing beds or sleeping areas
- Children in daycare settings
- Residents and staff in nursing homes or other care facilities
Indirect Transmission Through Objects
While less common, scabies can sometimes spread through contaminated items such as clothing, bedding, or towels. However, mites can only survive away from human skin for 48-72 hours under normal conditions, making this type of transmission less likely than direct contact.
Risk Factors That Increase Spread
Several conditions make scabies transmission more likely:
Overcrowded Living Conditions: When people live in close quarters with limited space, the chances of prolonged skin contact increase significantly.
Institutional Settings: Places like nursing homes, prisons, hospitals, and refugee camps provide ideal conditions for scabies outbreaks due to close contact between residents and staff.
War and Crisis Situations: During conflicts or natural disasters, displacement and crowded temporary housing create perfect conditions for scabies transmission.
Shared Sleeping Arrangements: Sharing beds or bedrooms significantly increases transmission risk due to prolonged contact during sleep when mites are most active.
Recognizing the Signs and Symptoms
The Hallmark Symptom: Intense Itching
The most characteristic feature of scabies is severe itching that becomes worse at night. This nocturnal pattern occurs because mites are more active in warm conditions, and body temperature naturally rises under bedcovers. The itching can be so intense that it disrupts sleep and daily activities.
Importantly, the itching doesn’t start immediately after infection. In first-time infections, it typically takes 3-4 weeks for symptoms to develop as the body’s immune system learns to recognize the mites as foreign invaders. However, if someone has had scabies before, symptoms can appear within 24-48 hours due to the body’s immunological memory.
The Telltale Sign: Scabies Burrows
Burrows are the most specific sign of scabies and represent the actual tunnels that female mites create in the skin. These appear as thin, slightly raised, wavy lines that are grayish or skin-colored, typically measuring 5-15 millimeters long. At one end of the burrow, there may be a small bump or blister where the mite currently resides.
Unfortunately, burrows are often difficult to see because scratching and secondary skin changes can obscure them. They’re most commonly found in areas where the skin is thin and has few hair follicles.

Where Scabies Typically Appears
Scabies has predictable patterns of where it affects the body:
Most Common Areas in Adults:
- Between fingers (finger webs)
- Sides of fingers
- Wrists and forearms
- Elbows
- Armpits
- Around the navel
- Lower abdomen
- Genitals (especially in men)
- Inner thighs
- Feet, particularly the arch area
Different Patterns in Children and Infants: Unlike adults, babies and young children often develop scabies on areas typically spared in older individuals:
- Face and scalp
- Palms of hands
- Soles of feet
- All over the body
This difference occurs because children have thinner skin and different immune responses compared to adults.
Secondary Problems That Develop
Skin Damage from Scratching
The intense itching leads to persistent scratching, which creates additional skin problems:
Scratch Marks and Sores: Constant scratching creates small, crusted lesions that can become the most visible sign of the condition.
Bacterial Infections: Open wounds from scratching provide entry points for bacteria, leading to:
- Impetigo (superficial bacterial infection)
- Cellulitis (deeper skin infection)
- Abscess formation
- In severe cases, blood poisoning
Inflammatory Skin Changes
The body’s immune response to mites causes various types of skin inflammation:
Eczema-like Changes: The skin may become red, swollen, and scaly, resembling other skin conditions like atopic dermatitis.
Persistent Nodules: Some people develop firm, itchy bumps that can last for weeks or months after successful treatment, particularly in the groin area and armpits.
Special Forms of Scabies
Crusted (Norwegian) Scabies
This severe form of scabies occurs in people with weakened immune systems, such as those with HIV/AIDS, cancer patients receiving chemotherapy, or elderly individuals with dementia. Instead of the usual 10-15 mites found in regular scabies, crusted scabies patients may harbor thousands or even millions of mites.
The condition appears as thick, crusty patches of skin that may be mistaken for other conditions like psoriasis. Paradoxically, these patients often experience little to no itching due to their compromised immune response. However, they are extremely contagious and can easily spread scabies to healthcare workers and family members.
How Doctors Diagnose Scabies
Clinical Recognition
Most scabies cases are diagnosed based on the classic combination of:
- Intense itching, especially at night
- Characteristic distribution of lesions
- Similar symptoms in household members or close contacts
- Response to anti-scabies treatment
Laboratory Confirmation
When possible, doctors may confirm the diagnosis by:
Skin Scraping Examination: A small sample of skin is scraped from a suspected burrow and examined under a microscope to look for mites, eggs, or mite droppings. However, this test is only positive in 10-50% of cases, even when scabies is definitely present.
Dermoscopy: This technique uses a special magnifying device to look for the “jet with contrail” sign – the dark mite body with its burrow trail visible as a lighter line.
Conditions That Can Look Like Scabies
Several other conditions can cause similar symptoms:
- Eczema or atopic dermatitis
- Contact dermatitis from allergens or irritants
- Insect bite reactions
- Bacterial skin infections
- Drug reactions
- Other causes of chronic itching
Treatment Options That Work
Topical Medications (Applied to Skin)
Permethrin 5%: This is the gold standard treatment recommended by the World Health Organization. It’s highly effective and safe for most people, including pregnant women and children over 2 months old.
Benzyl Benzoate: A cost-effective alternative that’s widely available but may cause more skin irritation.
Sulfur cream : The safest option for pregnant women and very young infants, though it has an unpleasant smell.
Malathion: Effective but less commonly available, with some concerns about toxicity.
Lindane: Once popular but now rarely used due to potential nervous system toxicity.
Oral Medications
Ivermectin: This pill represents a major advance in scabies treatment. Given as a single dose based on body weight, it’s particularly useful for:
- Treating large numbers of people during outbreaks
- Patients who can’t apply topical treatments
- Crusted scabies cases
- Treatment failures with topical therapy
How to Apply Treatment Correctly
Success depends on proper application technique:
Timing: Apply medication at night when mites are most active.
Coverage: Apply from the neck down to cover all skin surfaces, including between fingers and toes and under fingernails.
Duration: Leave the medication on for 8-14 hours (overnight) before washing off.
Repeat Treatment: Apply a second dose after 7-14 days to kill newly hatched mites.
Treat Everyone: All household members and close contacts must be treated at the same time, even if they don’t have symptoms.
Essential Steps for Successful Treatment
Environmental Cleaning
Wash Items in Hot Water: Clothing, bedding, and towels used in the 72 hours before treatment should be washed in water hotter than 60°C (140°F) and dried on high heat.
Bag Non-Washable Items: Items that can’t be washed should be sealed in plastic bags for 72 hours to starve any mites.
Clean Living Spaces: While mites don’t survive long in the environment, vacuum carpets and furniture, and wash surfaces with standard cleaners.
Managing Expectations After Treatment
Continued Itching is Normal: Itching may persist for 2-4 weeks after successful treatment due to the body’s continued reaction to dead mites and their waste products.
Symptom Relief: Use oral antihistamines, soothing lotions, and mild topical steroids to manage post-treatment itching.
Follow-Up Care: See a healthcare provider if symptoms worsen or don’t improve after 4 weeks, as this may indicate treatment failure or reinfection.
Prevention and Control Measures
Individual Prevention
Avoid Prolonged Skin Contact: With known infected individuals until they’ve been treated for at least 24 hours.
Practice Good Hygiene: While scabies isn’t caused by poor hygiene, regular bathing and clean clothing help overall skin health.
Prompt Treatment: Seek medical attention quickly if symptoms develop, as early treatment prevents spread to others.
Community and Institutional Control
Outbreak Management: In settings like nursing homes or schools, coordinate simultaneous treatment of all potentially exposed individuals.
Education Programs: Teach healthcare workers, teachers, and community leaders to recognize scabies symptoms and transmission patterns.
Contact Tracing: Identify and treat all close contacts of infected individuals to break transmission chains.
Special Considerations for Different Groups
Children and Infants
- Require careful medication selection due to safety concerns
- May need treatment of face and scalp areas
- Often develop more widespread skin involvement
- Higher risk of secondary bacterial infections
Elderly and Immunocompromised Patients
- May develop atypical presentations with minimal itching
- Higher risk of crusted scabies
- Require isolation precautions in healthcare settings
- May need oral treatment in addition to topical therapy
Pregnant Women
- Limited to safest treatment options like permethrin or sulfur
- Require careful monitoring for secondary infections
- Need treatment of household contacts to prevent reinfection
Long-Term Outlook and Complications
With Proper Treatment
Scabies is completely curable when diagnosed correctly and treated appropriately. Most patients experience significant improvement within days of treatment, though complete resolution of itching may take several weeks.
Potential Complications of Untreated Scabies
Secondary Bacterial Infections: Can lead to more serious conditions like kidney problems (post-infectious glomerulonephritis) especially in children.
Psychological Impact: Chronic itching and visible skin lesions can cause anxiety, depression, and social isolation.
Community Outbreaks: Untreated cases can lead to widespread transmission in households, schools, and institutions.
Global Health Impact
Scabies affects an estimated 200-300 million people worldwide at any given time. It’s particularly common in:
- Tropical and subtropical regions
- Overcrowded urban areas
- Resource-limited communities
- Areas affected by conflict or natural disasters
The World Health Organization has recognized scabies as a neglected tropical disease, highlighting the need for increased attention and resources for prevention and control programs.
Key Messages for Patients and Families
Scabies is Completely Curable: With proper diagnosis from dermatologist and treatment, scabies can be eliminated entirely.
Education is Crucial: Understanding how scabies spreads and how to prevent reinfection is essential for successful treatment.
Everyone Must Be Treated: All household members and close contacts need treatment at the same time, even without symptoms.
Don’t Be Embarrassed: Scabies can affect anyone regardless of cleanliness or social status – it’s simply a contagious condition that requires medical treatment.
Follow Instructions Carefully: Success depends on proper application of medications and completion of the full treatment course.
The successful management of scabies requires a comprehensive approach that combines accurate diagnosis, appropriate treatment, thorough contact management, and patient education. When these elements come together, this ancient condition can be completely eliminated, allowing patients to return to normal, comfortable lives free from the burden of persistent itching and skin irritation.

