Introduction
Melasma, derived from the Greek word meaning “a black spot,” represents one of the most challenging pigmentary disorders encountered in dermatological practice. This acquired hyperpigmentation condition, also known as chloasma or the “mask of pregnancy,” affects millions of individuals worldwide, predominantly women of reproductive age. Understanding the complex pathophysiology, accurate diagnosis, and evidence-based treatment approaches is crucial for dermatologists and healthcare providers managing this cosmetically distressing condition.
Definition and Clinical Characteristics
Melasma manifests as acquired light to dark brown hyperpigmented macules and patches that occur primarily on sun-exposed areas of the face. The condition is characterized by its symmetric distribution, serrated geographic borders, and tendency to coalesce into reticular patterns. The pigmentation can range from light brown to black, with color uniformity varying between patients and even within individual lesions.
According to the World Health Organization’s classification of skin disorders, melasma falls under acquired disorders of pigmentation and significantly impacts quality of life due to its cosmetic implications. The condition typically presents in three distinct facial patterns: centrofacial (affecting the forehead, cheeks, nose, and upper lip), malar (involving the cheeks and nose), and mandibular (affecting the jawline and chin).
Epidemiology and Risk Factors
Melasma demonstrates a striking female predominance, with studies indicating a 90:10 female-to-male ratio. The condition primarily affects women between the ages of 20-40 years, coinciding with reproductive years. Research published in the Journal of the American Academy of Dermatology indicates that melasma affects approximately 15-50% of pregnant women, earning it the colloquial term “pregnancy mask.”
Genetic predisposition plays a significant role, with studies showing that individuals with darker skin types (Fitzpatrick skin types III-V) are at higher risk. A family history of melasma is reported in 30-50% of cases, suggesting hereditary components. Geographic factors also contribute, with higher prevalence rates observed in tropical and subtropical regions where UV exposure is intense year-round.
Primary Precipitating Factors
Hormonal Influences: Estrogen and progesterone fluctuations represent the most significant triggers. Pregnancy-related melasma occurs in up to 70% of pregnant women, typically manifesting during the second and third trimesters. Oral contraceptive use and hormone replacement therapy are associated with melasma development in 10-25% of users.
UV Radiation Exposure: Ultraviolet radiation acts as both an initiating and exacerbating factor. UVA and UVB radiation stimulate melanocyte activity and increase melanin production. Studies demonstrate that even minimal sun exposure can trigger melasma recurrence in susceptible individuals.
Additional Risk Factors: Other contributing factors include certain medications (antiepileptics, heavy metals, amiodarone), cosmetic products containing phototoxic ingredients, nutritional deficiencies, psychological stress, and thyroid dysfunction.
Pathophysiology and Melanin Biology
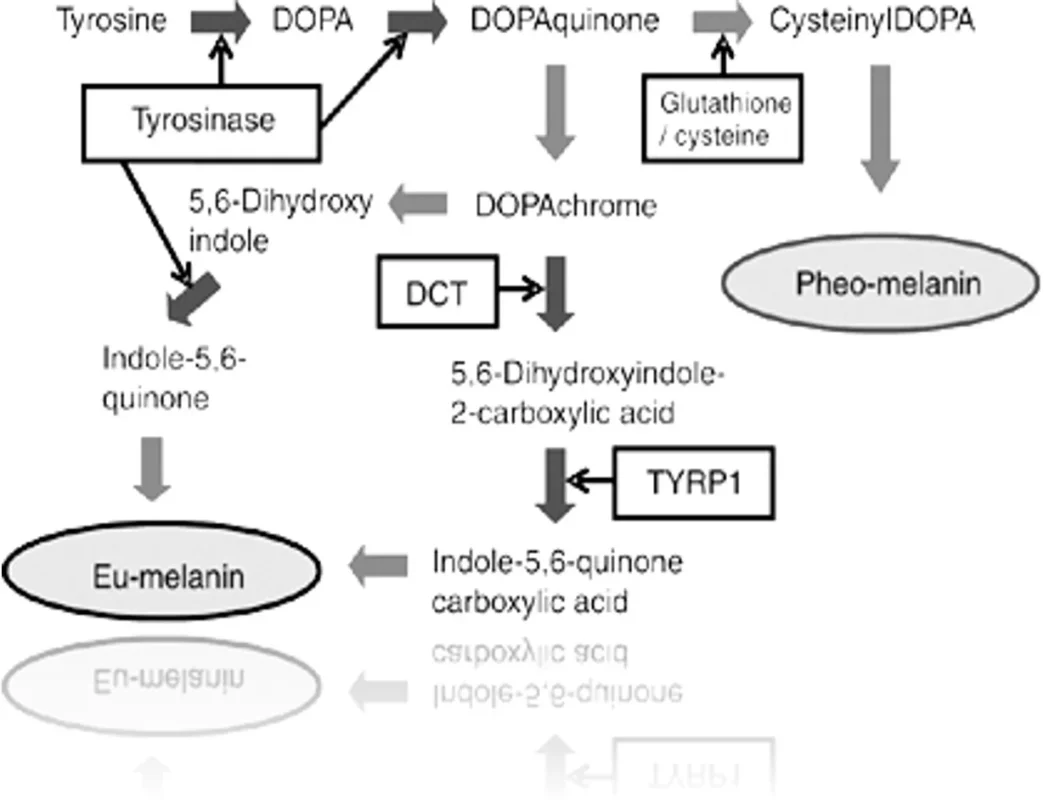
The pathogenesis of melasma involves complex interactions within the melanocyte-epidermal unit. Normal melanin synthesis occurs through the tyrosinase-mediated conversion of tyrosine to DOPA (3,4-dihydroxyphenylalanine), followed by oxidation to dopaquinone and subsequent formation of eumelanin and pheomelanin.
In melasma, this process becomes dysregulated, leading to increased melanin production and altered distribution. The condition can be classified histologically into three types:
- Epidermal Melasma: Characterized by increased melanin production and enlarged melanocytes in the epidermis
- Dermal Melasma: Involving melanin-containing macrophages (melanophages) in the dermis
- Mixed Type: Combining features of both epidermal and dermal involvement
Recent research published in Pigment Cell & Melanoma Research has identified additional factors beyond UV exposure, including vascular changes, basement membrane alterations, and inflammatory mediators that contribute to melasma development and persistence.
Diagnostic Evaluation
Clinical Assessment
Comprehensive evaluation begins with detailed history-taking, focusing on onset, duration, precipitating factors, and previous treatments. Physical examination should document the distribution pattern, color intensity, and morphological characteristics of the lesions.
Wood’s Lamp Examination
Wood’s lamp examination using 365nm ultraviolet light provides crucial diagnostic information and helps classify melasma subtypes:
- Epidermal melasma: Shows enhancement and accentuation under Wood’s lamp
- Dermal melasma: Demonstrates no enhancement
- Mixed type: Shows enhancement without significant accentuation
- Very dark skin: May not show visible changes under Wood’s lamp
Laboratory Investigations
Laboratory testing is generally unnecessary unless clinical history suggests underlying endocrinopathies. When indicated, thyroid function tests, liver function assessment, and hormonal evaluations may be performed.
Evidence-Based Treatment Modalities
Photoprotection: The Foundation of Management
Broad-spectrum sunscreen use represents the cornerstone of melasma management. According to the American Academy of Dermatology guidelines, sunscreens should provide protection against both UVA and UVB radiation with an SPF of at least 30. Physical sunscreens containing zinc oxide and titanium dioxide are preferred due to their broad-spectrum coverage and minimal skin irritation.
Studies published in the Journal of Cosmetic Dermatology demonstrate that consistent sunscreen use can prevent melasma progression and enhance treatment efficacy when combined with depigmenting agents.
Topical Depigmenting Agents
Hydroquinone: Considered the gold standard for melasma treatment, hydroquinone (2-4%) functions as a tyrosinase inhibitor, reducing melanin synthesis. Clinical trials show 60-80% improvement rates with 12-24 weeks of treatment. However, prolonged use may lead to exogenous ochronosis, particularly in darker skin types.
Tretinoin: This vitamin A derivative (0.025-0.1%) enhances epidermal turnover and facilitates melanin dispersal. Studies indicate that tretinoin alone provides modest improvement but significantly enhances efficacy when combined with hydroquinone.
Azelaic Acid: Available in 15-20% concentrations, azelaic acid selectively inhibits hyperactive melanocytes while sparing normal cells. Research published in the International Journal of Dermatology shows comparable efficacy to hydroquinone with fewer side effects.
Kojic Acid: Derived from fungal sources, kojic acid (1-4%) inhibits tyrosinase activity. Studies demonstrate moderate efficacy with good tolerability profiles.
Combination Therapies
The Kligman formula, combining hydroquinone (4%), tretinoin (0.05%), and a mild corticosteroid (fluocinolone acetonide 0.01%), represents the most studied combination therapy. Clinical trials published in the Archives of Dermatology show superior efficacy compared to individual components, with 60-80% of patients achieving significant improvement within 8-12 weeks.
Chemical Peels
Superficial chemical peels accelerate epidermal turnover and enhance penetration of topical agents. Glycolic acid (30-70%), salicylic acid (20-30%), and lactic acid peels show efficacy in clinical studies. A systematic review in Dermatologic Surgery indicates that combination therapy with peels and topical agents provides superior results compared to monotherapy.

Advanced Therapies
Laser and Light-Based Treatments: Q-switched lasers (Nd:YAG 1064nm, Ruby 694nm) target melanin-containing structures. However, studies show variable results with significant risk of post-inflammatory hyperpigmentation, particularly in darker skin types.
Intense Pulsed Light (IPL): Delivers broad-spectrum light (515-1200nm) with moderate efficacy. Clinical trials show 40-60% improvement rates with multiple sessions.
Fractional Photothermolysis: Creates microscopic thermal zones to promote melanin removal. Studies indicate promising results with reduced downtime compared to traditional resurfacing.
Patient Education and Lifestyle Modifications
According to WHO guidelines for chronic disease management, patient education forms a critical component of melasma treatment. The “triad” approach emphasizing sunprotection, bleaching agents, and time remains fundamental. Patients should understand that melasma is a chronic condition requiring long-term management and that results are gradual, typically becoming apparent after 3-6 months of consistent treatment.
Key educational points include:
- Daily broad-spectrum sunscreen application
- Use of protective clothing and wide-brimmed hats
- Avoidance of known triggers
- Realistic expectations regarding treatment timeline
- Importance of treatment compliance
Treatment Protocols and Clinical Recommendations
Morning Regimen
- Gentle cleansing with alpha-hydroxy acid-containing cleanser
- Application of depigmenting agent (hydroquinone, kojic acid, or azelaic acid)
- Broad-spectrum sunscreen (SPF ≥30)
- Physical protection measures
Evening Regimen
- Gentle cleansing
- Retinoid application (tretinoin or adapalene)
- Moisturization as needed
Professional Treatments
Biweekly chemical peels (glycolic or salicylic acid) with gradually increasing concentrations based on tolerance. Some practitioners recommend microdermabrasion prior to chemical peels to enhance penetration.
Topical Depigmenting Agents: Available at Derma.pk
Hydroquinone-Based Products
Hydroquinone remains the gold standard for melasma treatment, functioning as a competitive inhibitor of tyrosinase enzyme. Available products include:
Available at Derma.pk:
- Hydroquinone Cream for Melasma: Professional-grade formulations typically containing 2-4% hydroquinone with enhanced stability and penetration enhancers.
Mechanism of Action: Hydroquinone works through multiple pathways:
- Competitive inhibition of tyrosinase enzyme
- Destruction of melanosomes and melanocytes
- Inhibition of DNA and RNA synthesis in melanocytes
- Reduction of melanin polymer formation
Clinical Efficacy: Multiple randomized controlled trials demonstrate:
- 60-80% improvement rates with 12-24 weeks of treatment
- Superior efficacy when combined with tretinoin and corticosteroids
- Sustained improvement with maintenance therapy
Safety Considerations: Long-term use may lead to:
- Exogenous ochronosis (rare but permanent complication)
- Contact dermatitis and skin irritation
- Rebound hyperpigmentation upon discontinuation
- Nail discoloration with prolonged use
Tretinoin and Retinoid Products
Available at Derma.pk:
- COSMED Cream for Skin Fairness | Q10 Retinol & Dark Spot Reducer: Combines retinol with coenzyme Q10 for enhanced antioxidant protection and cellular regeneration.
Mechanism of Action: Retinoids enhance melasma treatment through:
- Acceleration of epidermal turnover
- Facilitation of melanin dispersal
- Enhancement of topical agent penetration
- Normalization of melanocyte function
- Anti-inflammatory effects
Clinical Evidence: Studies published in Archives of Dermatology show:
- Modest efficacy as monotherapy (30-40% improvement)
- Synergistic effects when combined with hydroquinone
- Enhanced penetration of other depigmenting agents
- Long-term benefits for skin texture and quality
Azelaic Acid Formulations
Available at Derma.pk:
- Azelaic Acid Plus Clindamycin Cream – for Acne & Pigmentation: Dual-action formulation addressing both pigmentation and inflammatory components.
Mechanism of Action: Azelaic acid provides selective melanocyte inhibition through:
- Competitive inhibition of tyrosinase
- Selective cytotoxicity to hyperactive melanocytes
- Anti-inflammatory properties
- Normalization of keratinization
- Antimicrobial effects against Propionibacterium acnes
Clinical Advantages: Research demonstrates:
- Comparable efficacy to 2% hydroquinone
- Excellent safety profile with minimal side effects
- Suitable for long-term maintenance therapy
- Safe during pregnancy and lactation
- Additional benefits for acne and rosacea
Glycolic Acid and Alpha Hydroxy Acid Products
Available at Derma.pk:
- Glyjic-A Cream – Melasma Treatment & Skin Lightening: Professional formulation combining glycolic acid with other depigmenting agents.
Mechanism of Action: Alpha hydroxy acids work through:
- Acceleration of epidermal turnover
- Removal of pigmented corneocytes
- Enhancement of topical agent penetration
- Stimulation of collagen synthesis
- Improvement of skin texture and tone
Clinical Applications: Studies show:
- Effective as adjunctive therapy
- Enhanced penetration of hydroquinone and tretinoin
- Improvement in skin texture and photodamage
- Suitable for combination with chemical peels
Advanced Combination Formulations
Available at Derma.pk:
- Emerence Melasma Care KATxa – Removes Dark Spots & Freckles: Advanced formulation likely containing multiple active ingredients for comprehensive melasma management.
Tranexamic Acid-Based Products
Available at Derma.pk:
- TXA Serum with Niacinamide & Zinc – Hyperpigmentation & Dark Circle Treatment: Innovative formulation combining tranexamic acid with niacinamide for enhanced efficacy.
Mechanism of Action: Tranexamic acid provides unique benefits through:
- Inhibition of plasmin activation
- Reduction of prostaglandin E2 production
- Decreased melanocyte activation
- Anti-inflammatory effects
- Improvement in vascular component of melasma
Clinical Evidence: Recent studies demonstrate:
- Significant improvement in melasma severity
- Reduced recurrence rates
- Excellent safety profile
- Synergistic effects with traditional treatments
Vitamin C and Antioxidant Serums
Available at Derma.pk:
- THE PUREST SOLUTION (20% ASCORBIC ACID AND 0.5% FERULIC ACID) VITAMIN C BRIGHTENING AND LIGHTENING SERUM 30ML: High-concentration vitamin C with stabilizing ferulic acid.
Mechanism of Action: Vitamin C provides multiple benefits:
- Antioxidant protection against UV-induced damage
- Inhibition of tyrosinase enzyme activity
- Reduction of melanin synthesis
- Enhancement of collagen synthesis
- Protection against environmental oxidative stress
Clinical Benefits: Research demonstrates:
- Modest depigmenting effects
- Significant photoprotective benefits
- Enhanced efficacy when combined with other treatments
- Improvement in overall skin quality and radiance
Arbutin-Based Formulations
Available at Derma.pk:
- THE PUREST SOLUTION ARBUTIN 2%+HYALURONIC ACID BRIGHTENING SERUM | 30ml: Natural depigmenting agent with hydrating benefits.
Mechanism of Action: Arbutin works through:
- Competitive inhibition of tyrosinase
- Gradual release of hydroquinone
- Gentle depigmenting action
- Hydrating and soothing properties
Clinical Advantages: Studies show:
- Gentle action suitable for sensitive skin
- Reduced risk of irritation compared to hydroquinone
- Natural origin appealing to many patients
- Good long-term safety profile
Sunblocks with High Sun Protection Factor
- Sunpaly skin aqua sunblock SPF 50
- Radiant ultra SPF 60 sunblock
- Solarin 60
- Skintelligent high protection SPF 60
Prognosis and Long-term Management
Melasma prognosis varies significantly based on etiology and treatment compliance. Pregnancy-related melasma may improve spontaneously postpartum, with studies showing complete resolution in 30-50% of cases within one year. However, hormone-independent melasma typically requires ongoing treatment for maintenance of improvement.
Long-term studies published in the Journal of the European Academy of Dermatology indicate that consistent photoprotection and maintenance therapy with low-concentration depigmenting agents can prevent recurrence in 70-80% of patients.
Conclusion
Melasma management requires a comprehensive, individualized approach combining evidence-based therapies with patient education and lifestyle modifications. While complete cure remains elusive, significant improvement is achievable through consistent treatment protocols emphasizing photoprotection, appropriate depigmenting agents, and patient compliance. Future research directions include novel therapeutic targets, improved combination formulations, and personalized treatment approaches based on genetic and molecular markers.
Success in melasma management depends on realistic patient expectations, consistent treatment adherence, and long-term commitment to photoprotection. As our understanding of melasma pathophysiology continues to evolve, treatment outcomes are expected to improve, offering hope for the millions of individuals affected by this challenging condition.

