Dry Patches on Face: Eczema, Seborrheic Dermatitis, or Just Dry Skin?
Discovering dry, flaky patches on your face can be both concerning and frustrating. These patches may appear suddenly or develop gradually, creating rough, scaly areas that affect your skin’s appearance and comfort. Understanding whether you’re dealing with simple dry skin, eczema, or seborrheic dermatitis is crucial for selecting the right treatment approach and achieving clear, healthy skin.
In Pakistan’s diverse climate conditions, facial dry patches are increasingly common due to extreme weather variations, air pollution, and lifestyle factors. From Karachi’s humid coastal environment to Lahore’s dry winters and Islamabad’s seasonal changes, different regions present unique challenges for maintaining facial skin health.
This comprehensive guide will help you identify the specific cause of your facial dry patches, understand the underlying mechanisms, and discover effective treatment options available through professional dermatological care.
Understanding Facial Dry Patches: Medical Overview
Simple Dry Skin (Xerosis):
Dry skin represents the mildest form of facial dryness, typically resulting from environmental factors or inadequate skincare routines. Research shows that the skin’s natural moisture barrier can lose up to 25% of its hydration capacity during winter months or in low-humidity environments.
Clinical studies indicate that simple dry skin affects 40-60% of adults during seasonal transitions, with higher prevalence in urban areas due to pollution and indoor heating/cooling systems.
Eczema (Atopic Dermatitis):
Eczema is a chronic inflammatory skin condition affecting 10-20% of children and 1-3% of adults globally. Research published in the Journal of Allergy and Clinical Immunology demonstrates that facial eczema often presents differently from body eczema, with more subtle inflammation but significant impact on quality of life.
The condition involves complex interactions between genetic predisposition, immune dysfunction, and environmental triggers, with studies showing that 70% of patients have a family history of atopic diseases.
Seborrheic Dermatitis:
Seborrheic dermatitis affects 3-5% of the general population, with higher rates in certain demographics. Research indicates that this condition results from an inflammatory response to Malassezia yeasts, which proliferate in sebum-rich areas of the face.
Studies show that seborrheic dermatitis has a bimodal age distribution, with peaks in infancy and adults aged 30-60 years, particularly affecting men more than women.
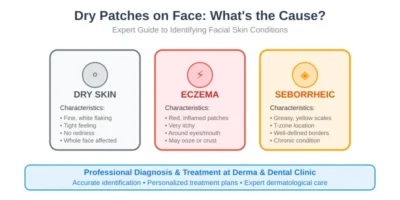
Visual Identification Guide
Simple Dry Skin Characteristics:
Appearance:
- Light flaking or scaling without significant redness
- Rough, tight sensation, especially after cleansing
- Fine lines may appear more prominent
- Skin appears dull or lackluster
Distribution:
- Often affects entire face uniformly
- May be more noticeable on cheeks and around eyes
- Typically doesn’t follow specific anatomical patterns
Associated Symptoms:
- Mild itching, particularly after washing
- Feeling of tightness or discomfort
- Improved with moisturizer application
- No significant inflammation or swelling
Eczema (Atopic Dermatitis) Identification:
Appearance:
- Red, inflamed patches with scaling
- May present as small bumps (papules) that can ooze
- Lichenification (thickened skin) from chronic scratching
- Color may range from pink to dark brown depending on skin tone
Distribution:
- Common around eyes, especially eyelids
- Frequently affects perioral area (around mouth)
- May involve forehead and temples
- Often asymmetrical distribution
Associated Symptoms:
- Intense itching, often worse at night
- Burning or stinging sensation
- Possible secondary bacterial infection from scratching
- Symptoms often triggered by stress, allergens, or weather changes
Seborrheic Dermatitis Recognition:
Appearance:
- Yellowish, greasy scales on red, inflamed base
- Well-demarcated patches with irregular borders
- Scales may appear “stuck on” to the skin
- Color ranges from pink to red with yellowish scaling
Distribution:
- Predominantly affects T-zone (forehead, nose, chin)
- Eyebrows and eyelash margins commonly involved
- Nasolabial folds (lines from nose to mouth corners)
- May extend to hairline and scalp margins
Associated Symptoms:
- Mild to moderate itching
- Burning sensation in some cases
- Worsening with stress, fatigue, or seasonal changes
- Often improves with antifungal treatments
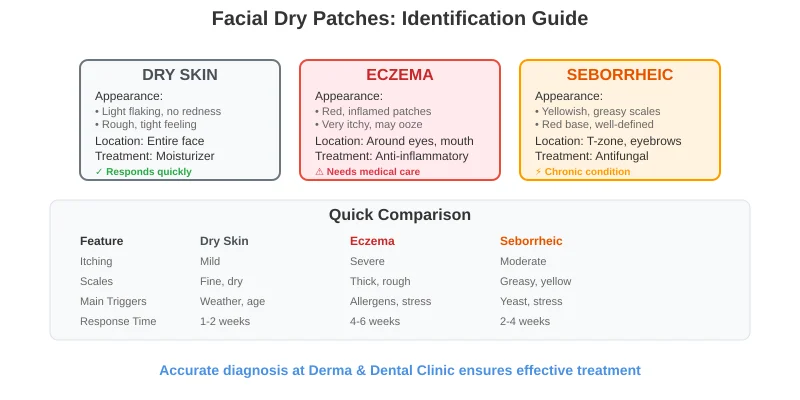
Comprehensive Differential Diagnosis
Diagnostic Criteria Comparison:
Simple Dry Skin:
- Onset: Gradual, seasonal correlation
- Triggers: Weather changes, over-cleansing, aging
- Response: Improves readily with moisturization
- Inflammatory signs: Minimal to none
Eczema (Atopic Dermatitis):
- Onset: Can be sudden or chronic
- Triggers: Allergens, stress, irritants, temperature changes
- Response: Requires anti-inflammatory treatment
- Inflammatory signs: Prominent redness, swelling, possible oozing
Seborrheic Dermatitis:
- Onset: Typically gradual, may have periodic flares
- Triggers: Stress, hormonal changes, weather, certain foods
- Response: Improves with antifungal treatments
- Inflammatory signs: Moderate inflammation with characteristic greasy scales
Laboratory and Clinical Assessment:
When Professional Evaluation is Needed: Research shows that accurate diagnosis requires professional assessment in 60-70% of cases due to overlapping presentations and potential for mixed conditions.
Diagnostic Tools:
- Patch testing: For identifying contact allergens in suspected allergic contact dermatitis
- KOH preparation: To rule out fungal infections
- Dermoscopy: For detailed examination of scale patterns and inflammation
- Biopsy: Rarely needed but may be indicated for atypical presentations
Environmental Factors in Pakistan:
- Low humidity: Winter months in northern Pakistan can drop humidity below 30%
- Air pollution: PM2.5 levels in major cities exceed WHO guidelines by 300-400%
- UV exposure: High altitude areas experience increased UV intensity
- Temperature extremes: Rapid temperature changes stress skin barrier function
Research published in Environmental Research shows that air pollution increases skin sensitivity by 40% and disrupts normal barrier function.
Lifestyle Factors:
- Over-cleansing: Using harsh soaps or cleansing more than twice daily
- Hot water exposure: Temperatures above 37°C strip natural oils
- Inadequate moisturization: Failure to apply moisturizer within 3 minutes of cleansing
- Wrong product selection: Using products inappropriate for skin type
Occupational Exposures:
- Healthcare workers: Frequent hand washing and alcohol-based sanitizers
- Outdoor workers: Excessive sun and wind exposure
- Industrial workers: Chemical exposure affecting skin barrier
Medical and Genetic Factors:
Systemic Conditions: Research indicates several medical conditions increase dry skin risk:
- Hypothyroidism: Affects 8-10% of Pakistani women, causing dry skin in 70% of cases
- Diabetes: Present in 26% of Pakistani adults, associated with skin barrier dysfunction
- Autoimmune conditions: Sjögren’s syndrome, lupus affecting skin moisture
Genetic Predisposition: Studies show that filaggrin gene mutations, present in 8-10% of South Asian populations, significantly increase eczema risk and skin barrier dysfunction.
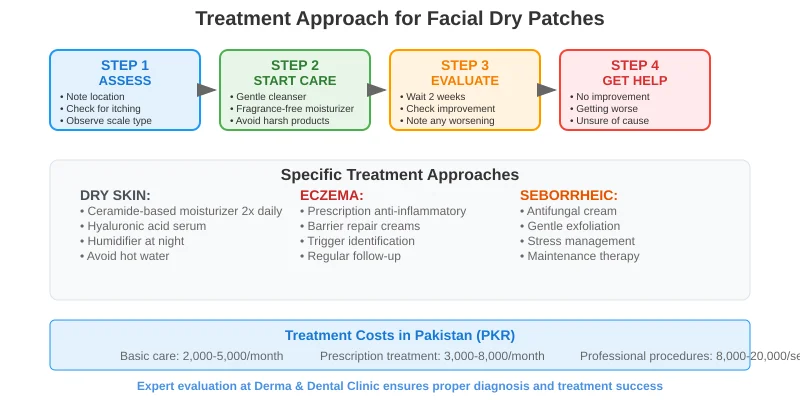
Comprehensive Treatment Protocols
Simple Dry Skin Management:
Immediate Relief Measures:
- Gentle cleansing: Use lukewarm water and mild, fragrance-free cleansers
- Moisturizer application: Within 3 minutes of cleansing while skin is damp
- Humidification: Maintain indoor humidity at 40-60%
- Sun protection: Daily SPF 30+ application
Product Recommendations: Research shows that ceramide-containing moisturizers improve skin barrier function by 35% within 2 weeks of consistent use.
Effective Ingredients:
- Hyaluronic acid: Holds 1000 times its weight in water
- Glycerin: Humectant properties draw moisture to skin
- Ceramides: Restore natural skin barrier
- Niacinamide: Reduces water loss and improves barrier function
Eczema (Atopic Dermatitis) Treatment:
Topical Therapy: Clinical trials show that early, consistent treatment prevents disease progression and reduces flare frequency by 50-70%.
First-Line Treatments:
- Topical corticosteroids: Hydrocortisone 1% for mild cases, stronger preparations for severe inflammation
- Calcineurin inhibitors: Tacrolimus or pimecrolimus for sensitive facial areas
- Barrier repair creams: Products containing physiological lipids and ceramides
Advanced Treatments Available at Derma & Dental Clinic:
- Prescription moisturizers: Medical-grade barrier repair formulations
- Phototherapy: Targeted UV treatment for chronic cases
- Systemic immunomodulators: For severe, widespread eczema
Maintenance Strategies:
- Daily moisturization with prescription-strength products
- Identification and avoidance of personal triggers
- Stress management techniques
- Regular follow-up care to prevent flares
Seborrheic Dermatitis Management
Antifungal Therapy: Research demonstrates that antifungal treatments show improvement in 80-90% of cases within 2-4 weeks.
Topical Antifungals:
- Ketoconazole 2% cream: Applied twice daily for 2-4 weeks
- Selenium sulfide: For maintenance therapy
- Ciclopirox: Alternative for ketoconazole-resistant cases
Anti-inflammatory Adjuncts:
- Mild topical corticosteroids: For acute flares (limited use on face)
- Calcineurin inhibitors: Safer long-term option for facial use
Advanced Treatment Options:
- Hydrafacial treatments: Combines cleansing, exfoliation, and hydration
- Chemical peels: Gentle lactic acid peels for improved skin texture
- LED light therapy: Anti-inflammatory treatment for eczematous conditions
- Microneedling with serums: Enhanced delivery of therapeutic ingredients
For Severe or Treatment-Resistant Cases:
- Prescription compounding: Custom formulations for individual needs
- Photodynamic therapy: For severe seborrheic dermatitis
- Immunosuppressive therapy: Systemic treatments for severe atopic dermatitis
Innovative Therapies:
Emerging Treatment Options: Research in dermatological therapeutics shows promising results for:
- JAK inhibitors: Topical formulations showing 60-70% improvement in moderate-to-severe eczema
- Microbiome therapy: Probiotic skincare products restoring healthy skin flora
- Barrier repair technology: Advanced ceramide and lipid formulations
Prevention Strategies
Morning Routine:
- Gentle cleansing with lukewarm water
- Pat dry, leaving skin slightly damp
- Apply appropriate treatment (if prescribed)
- Moisturizer application within 3 minutes
- Broad-spectrum sunscreen (SPF 30+)
Evening Routine:
- Remove makeup and pollutants with gentle cleanser
- Pat dry gently
- Apply treatment products as directed
- Heavier moisturizer for overnight repair
Weekly Maintenance:
- Gentle exfoliation (1-2 times weekly maximum)
- Deep moisturizing treatments
- Professional assessment if symptoms worsen
Environmental Management:
- Maintain humidity at 40-60% using humidifiers
- Avoid direct heat or air conditioning on face
- Use air purifiers to reduce allergen exposure
- Choose hypoallergenic bedding and pillowcases
- Wide-brimmed hats for sun protection
- Scarves or masks in dusty/polluted environments
- Immediate cleansing after outdoor exposure
- Reapplication of moisturizer as needed
Lifestyle Modifications:
Dietary Considerations: Research suggests that certain dietary factors may influence skin conditions:
- Anti-inflammatory foods: Omega-3 fatty acids, antioxidant-rich vegetables
- Hydration: 8-10 glasses of water daily, increased in hot weather
- Trigger identification: Food diary to identify personal dietary triggers
Stress Management: Studies show that stress increases cortisol levels, worsening eczema in 70% of patients:
- Regular exercise (with immediate post-workout cleansing)
- Meditation or relaxation techniques
- Adequate sleep (7-9 hours nightly)
- Professional counseling if needed
When to Seek Professional Help
Red Flag Symptoms:
- Sudden onset of widespread facial inflammation
- Signs of secondary bacterial infection (pustules, increasing redness)
- Eczema herpeticum (clustered vesicles, especially around eyes)
- Failure to improve with appropriate treatment after 2-4 weeks
Routine Dermatological Assessment
Schedule Professional Evaluation When:
- Uncertain about diagnosis despite self-assessment
- Symptoms interfere with daily activities or sleep
- Cosmetic concerns affecting self-confidence
- Need for prescription treatments or professional procedures
- Desire for prevention-focused skincare planning
Visit Derma & Dental Clinic for comprehensive facial skin evaluation, accurate diagnosis, and personalized treatment plans using advanced dermatological techniques and proven protocols.
Treatment Success Rates:
- Simple dry skin: 90-95% complete resolution with appropriate care
- Atopic dermatitis: 70-80% achieve good control with maintenance therapy
- Seborrheic dermatitis: 80-90% improvement with antifungal treatment, requires ongoing maintenance
Quality of Life Impact:
Research shows that effective treatment of facial skin conditions significantly improves:
- Self-confidence and social interactions (85% of patients report improvement)
- Work performance and professional relationships
- Sleep quality (60% reduction in sleep disruption)
- Overall mental health and well-being
Long-term Management Success Factors:
- Consistent daily skincare routine
- Regular professional follow-up care
- Environmental modification and trigger avoidance
- Patient education and self-advocacy skills
Conclusion:
Identifying the cause of facial dry patches requires careful observation of symptoms, understanding of personal triggers, and often professional evaluation for accurate diagnosis. While simple dry skin, eczema, and seborrheic dermatitis may appear similar initially, their underlying causes, progression patterns, and treatment requirements differ significantly.
Pakistan’s diverse climate and environmental challenges make professional guidance particularly valuable for achieving optimal skin health. Early, accurate diagnosis combined with appropriate treatment prevents complications, reduces long-term healthcare costs, and maintains both skin health and quality of life.
The key to successful management lies in understanding your specific condition, implementing appropriate treatment protocols, and maintaining consistent care routines tailored to your individual needs and Pakistan’s unique environmental factors.
If you’re experiencing persistent facial dry patches or uncertainty about your diagnosis, consult with our experienced dermatologists at Derma & Dental Clinic. We provide comprehensive skin evaluations, accurate diagnoses, and personalized treatment plans designed for optimal results in Pakistan’s challenging environmental conditions.
Book your consultation today to receive expert care and develop a customized skincare strategy that addresses your specific concerns while preventing future complications.