Fungal Acne vs. Regular Acne: Why Your Breakouts Won’t Go Away
If you’ve been diligently following skincare routines, using acne treatments, and yet your breakouts persist or even worsen, you might be dealing with a commonly misdiagnosed condition: fungal acne. This frustrating skin condition masquerades as traditional acne but requires completely different treatment approaches, explaining why conventional acne therapies often fail to provide relief.
In Pakistan’s humid climate, where temperatures frequently exceed 35°C and humidity levels can reach 80%, fungal acne has become increasingly prevalent. The combination of heat, moisture, and lifestyle factors creates ideal conditions for Malassezia yeast overgrowth, leading to persistent breakouts that confuse both patients and healthcare providers.
Understanding the fundamental differences between fungal acne and regular acne is crucial for achieving clear skin and avoiding months of ineffective treatments that may actually exacerbate the condition.
Understanding the Pathophysiology
Regular Acne (Acne Vulgaris): Bacterial Origin
Regular acne results from a complex interaction of four primary factors affecting the pilosebaceous unit. Research published in the Journal of Clinical and Aesthetic Dermatology demonstrates that traditional acne involves Cutibacterium acnes (formerly Propionibacterium acnes) bacterial proliferation within clogged hair follicles.
The Traditional Acne Cascade:
- Sebaceous hyperactivity: Hormonal stimulation increases oil production by 300-500%
- Follicular hyperkeratinization: Abnormal skin cell shedding creates microcomedones
- Bacterial colonization: C. acnes proliferates in anaerobic, lipid-rich environments
- Inflammatory response: Bacterial byproducts trigger immune activation and visible lesions
Clinical studies indicate that hormonal fluctuations account for 70-80% of acne cases, with genetic predisposition contributing significantly to severity and persistence.
Fungal Acne (Malassezia Folliculitis): Yeast Overgrowth
Fungal acne represents a fundamentally different pathological process involving Malassezia species overgrowth within hair follicles. Research in Medical Mycology shows that this lipophilic yeast naturally inhabits human skin but can proliferate excessively under specific conditions.
The Fungal Acne Process:
- Environmental triggers: Heat, humidity, and occlusion promote yeast multiplication
- Follicular invasion: Malassezia organisms colonize hair follicle openings
- Inflammatory cascade: Yeast metabolites trigger immune responses
- Persistent inflammation: Creates characteristic uniform papular eruptions
Studies demonstrate that Malassezia folliculitis affects 45-60% more individuals in tropical and subtropical climates, making it particularly relevant for Pakistan’s population.
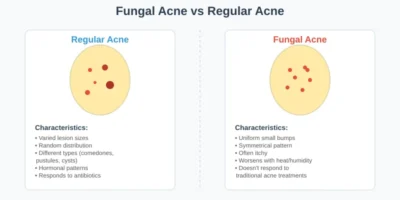
Comprehensive Differential Diagnosis
Regular Acne Identification:
Lesion Morphology:
- Diverse lesion types: Comedones, papules, pustules, nodules, and cysts
- Varied sizes: From 1-2mm comedones to 1-2cm cystic lesions
- Random distribution: Asymmetrical patterns with clustering tendencies
- Color variation: From skin-colored comedones to deep red inflammatory nodules
Clinical Presentation:
- Age correlation: Onset typically during puberty, may persist into adulthood
- Hormonal patterns: Premenstrual flares in 65% of women
- Seasonal variation: Often improves with controlled sun exposure
- Treatment response: Generally improves with antibacterial and anti-inflammatory therapies
Fungal Acne Characteristics:
Lesion Morphology:
- Monomorphic appearance: Uniform, small papules and pustules (1-3mm)
- Consistent presentation: Similar size and appearance across affected areas
- Symmetrical distribution: Even patterns on chest, back, and sometimes face
- Color uniformity: Typically red to pink inflammatory papules
Clinical Presentation:
- Environmental correlation: Worsens with heat, humidity, and sweating
- Activity association: Flares after exercise, hot weather, or occlusive clothing
- Treatment resistance: No improvement or worsening with conventional acne treatments
- Pruritic component: Often accompanied by itching, unlike typical acne
Anatomical Distribution Patterns:
Regular Acne Distribution: Research shows that traditional acne follows sebaceous gland density patterns:
- Facial involvement: T-zone predominance (forehead, nose, chin)
- Truncal patterns: Upper chest and back, often with larger lesions
- Age-related shifts: Adult acne often concentrates on jawline and lower face
Fungal Acne Distribution: Studies indicate that Malassezia folliculitis shows distinct preferences:
- Chest and upper back: Most common presentation sites (85% of cases)
- Shoulder involvement: Extending to deltoid regions
- Facial sparing: Less commonly affects face compared to regular acne
- Uniform density: Even distribution within affected areas
Microscopic and Laboratory Differentiation:
Diagnostic Confirmation Methods:
- KOH preparation: Direct microscopic examination reveals Malassezia spores and hyphae
- Fungal culture: Specialized media can isolate and identify Malassezia species
- Dermoscopy: Reveals characteristic follicular plugging patterns
- Response to antifungal therapy: Diagnostic trial often confirms suspicion
Research indicates that clinical diagnosis alone has 60-70% accuracy, while microscopic confirmation increases diagnostic certainty to 95%.
Evidence-Based Risk Factors and Triggers:
Environmental and Climate Factors:
- High humidity: Monsoon seasons create optimal Malassezia growth conditions
- Temperature extremes: Summer temperatures exceeding 40°C promote sweating
- Air pollution: Urban environments may compromise skin barrier function
- Lifestyle factors: Increased air conditioning use leading to rapid temperature changes
Research published in Dermatology Online Journal demonstrates that tropical climates increase fungal acne incidence by 300-400% compared to temperate regions.
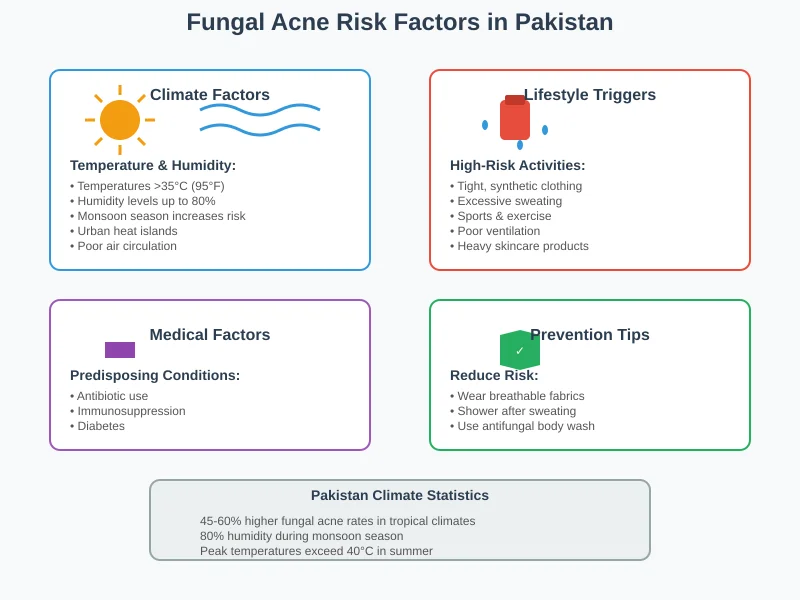
Lifestyle and Occupational Triggers:
- Athletic participation: Prolonged sweating in occlusive sportswear
- Occupational exposure: Kitchen workers, healthcare professionals in protective equipment
- Fashion choices: Tight, non-breathable clothing and synthetic fabrics
- Skincare practices: Over-moisturizing and occlusive product use
Medical and Pharmaceutical Triggers:
- Antibiotic therapy: Disrupts normal bacterial flora, allowing yeast overgrowth
- Immunosuppression: Corticosteroid use or systemic immunocompromise
- Hormonal fluctuations: Pregnancy, oral contraceptives, or endocrine disorders
- Dietary factors: High-carbohydrate diets may promote yeast proliferation
Skincare-Related Precipitants:
Product-Related Triggers: Research shows that certain skincare ingredients can exacerbate fungal acne:
- Fatty acids and esters: Oleic acid, lauric acid, and derivatives feed Malassezia
- Occlusive ingredients: Petrolatum, mineral oil creating anaerobic conditions
- Fermented ingredients: Some Asian beauty products may worsen fungal conditions
- Heavy moisturizers: Excessive hydration creating humid microenvironments
Studies indicate that 40-50% of fungal acne cases have identifiable skincare trigger factors.
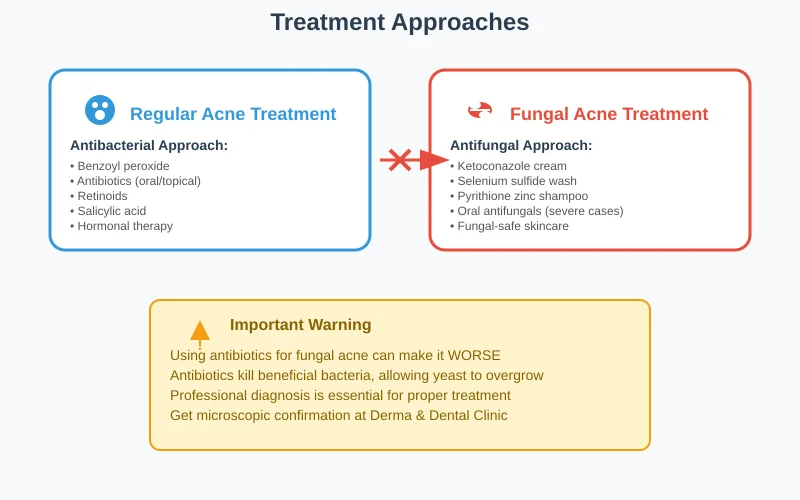
Comprehensive Treatment Protocols:
Regular Acne Management:
Topical Therapy Hierarchy: Clinical guidelines recommend stepwise approach based on severity:
First-Line Treatments:
- Benzoyl peroxide 2.5-10%: Reduces C. acnes by 99% within two weeks
- Topical retinoids: Adapalene, tretinoin, or tazarotene for comedonal control
- Salicylic acid 0.5-2%: Beta-hydroxy acid with anti-inflammatory properties
- Combination products: Benzoyl peroxide + retinoid or antibiotic combinations
Second-Line Options:
- Topical antibiotics: Clindamycin or erythromycin with benzoyl peroxide
- Azelaic acid 15-20%: Anti-inflammatory and antimicrobial properties
- Sulfur-based preparations: Traditional anti-inflammatory agents
Systemic Therapy Considerations:
- Oral antibiotics: Azithromycin, doxycycline, minocycline for moderate-to-severe cases
- Hormonal therapy: Oral contraceptives, spironolactone for women
- Isotretinoin: Reserved for severe, treatment-resistant cases
Fungal Acne Treatment Protocols:
Antifungal Therapy Approaches:
Topical Antifungal Treatments: Research demonstrates that topical antifungals show 80-90% efficacy in treating Malassezia folliculitis:
- Ketoconazole 2%: As directed by dermatologist.
- Selenium sulfide 2.5%: Used as body wash, left on for 10 minutes before rinsing
- Pyrithione zinc shampoo: Daily use on affected areas for 2-3 weeks
- Ciclopirox olamine: Alternative for ketoconazole-resistant cases
Systemic Antifungal Options:
- Fluconazole: 150-200mg weekly for 2-4 weeks
- Itraconazole: 200mg daily for 7-14 days
- Ketoconazole oral: Reserved for severe cases due to hepatotoxicity risk
Professional Treatment at Derma & Dental Clinic:
- Accurate diagnosis: Microscopic confirmation and expert evaluation
- Customized protocols: Tailored antifungal regimens based on severity
- Combination therapy: Strategic use of topical and systemic treatments
- Follow-up management: Monitoring response and preventing recurrence
Maintenance and Prevention Strategies:
- Intermittent antifungal therapy: Weekly treatments during high-risk periods
- Environmental modification: Reducing heat and humidity exposure
- Wardrobe adjustments: Breathable fabrics and loose-fitting clothing
- Skincare optimization: Fungal-safe product selection and routines
Laboratory Confirmation Methods:
Microscopic Examination:
- KOH preparation: Direct visualization of Malassezia organisms
- Calcofluor white staining: Enhanced fungal detection under fluorescence
- Gram staining: Reveals characteristic yeast morphology
Culture Techniques:
- Modified Dixon’s agar: Specialized medium for Malassezia isolation
- Sabouraud’s dextrose agar: With olive oil overlay for lipophilic yeasts
- Species identification: Determines specific Malassezia strain involvement
Molecular Diagnostics:
- PCR amplification: Rapid and specific Malassezia detection
- DNA sequencing: Definitive species identification
- Quantitative assessment: Determines organism load and treatment response
Dermoscopic Evaluation:
Characteristic Dermoscopic Features:
- Follicular plugging: White or yellow keratotic plugs in follicular openings
- Perifollicular erythema: Inflammatory halos around affected follicles
- Absence of comedones: Lack of typical blackheads and whiteheads
- Uniform distribution: Regular spacing of similar lesions
Research shows that dermoscopy increases diagnostic accuracy by 25-30% when combined with clinical assessment.
Why Conventional Acne Treatments Fail?
Antibacterial vs. Antifungal Requirements:
- Mechanism mismatch: Antibiotics may worsen fungal overgrowth
- Microbiome disruption: Killing beneficial bacteria allows yeast proliferation
- Inflammatory persistence: Continued yeast presence maintains inflammation
- Product feeding: Acne moisturizers often contain Malassezia-promoting ingredients
Common Treatment Errors: Studies indicate that 60-70% of fungal acne cases receive inappropriate initial treatment:
- Extended antibiotic courses: Worsening yeast overgrowth
- Aggressive exfoliation: Mechanical irritation promoting inflammation
- Heavy moisturizer use: Creating favorable yeast growth conditions
- Retinoid overuse: Initial irritation masking underlying fungal infection
Professional Intervention Benefits:
Expert Diagnosis Advantages:
- Microscopic confirmation: Eliminating diagnostic uncertainty
- Species identification: Targeting specific Malassezia strains
- Resistance testing: Guiding appropriate antifungal selection
- Comorbidity assessment: Identifying predisposing systemic conditions
Comprehensive Treatment Planning:
- Combination protocols: Optimizing topical and systemic approaches
- Timeline management: Realistic expectations and monitoring schedules
- Adjunctive therapies: Addressing inflammation and barrier repair
- Prevention strategies: Long-term maintenance and risk reduction
Prevention and Long-Term Management:
Climate Adaptation Strategies:
- Air conditioning optimization: Maintaining 60-70% humidity levels
- Clothing selection: Natural, breathable fabrics and loose fits
- Activity timing: Avoiding outdoor exercise during peak heat
- Post-exercise protocols: Immediate showering and clothing changes
Skincare Routine Optimization:
- Fungal-safe products: Avoiding Malassezia-feeding ingredients
- Minimal routine approach: Reducing product layering and occlusion
- pH balance maintenance: Using products that support healthy skin barrier
- Regular antifungal maintenance: Preventive treatments during high-risk periods
Professional Monitoring:
Follow-up Protocols:
- Response assessment: Monitoring improvement at 2, 4, and 8 weeks
- Maintenance planning: Developing long-term prevention strategies
- Recurrence management: Early intervention for breakthrough episodes
- Lifestyle counseling: Ongoing education about triggers and prevention
At Derma & Dental Clinic, we provide comprehensive fungal acne management including accurate diagnosis, effective treatment protocols, and long-term prevention strategies tailored to Pakistan’s challenging climate conditions.
Conclusion
Distinguishing between fungal acne and regular acne represents a critical diagnostic challenge with significant implications for treatment success and patient quality of life. The fundamental pathophysiological differences between bacterial acne and Malassezia folliculitis require completely different therapeutic approaches, explaining why conventional acne treatments often fail or worsen fungal conditions.
Pakistan’s climate creates particularly favorable conditions for fungal acne development, making professional expertise in differential diagnosis essential for optimal outcomes. The combination of high humidity, elevated temperatures, and lifestyle factors unique to the region necessitates specialized knowledge and experience in managing these challenging cases.
Key takeaways for patients experiencing persistent breakouts:
- Diagnostic accuracy matters: Professional evaluation can prevent months of ineffective treatment
- Treatment approach differs fundamentally: Antifungal therapy vs. antibacterial approaches
- Environmental factors play crucial roles: Climate and lifestyle modifications are essential
- Maintenance prevents recurrence: Long-term strategies ensure sustained improvement
- Quality of life improves dramatically: Appropriate treatment restores confidence and function
If your acne treatments aren’t working or your breakouts seem different from typical acne, schedule a consultation with our experienced dermatologists at Derma & Dental Clinic. We provide expert diagnosis using advanced microscopic techniques, personalized treatment protocols, and comprehensive management strategies designed specifically for Pakistan’s unique environmental challenges.
Don’t waste more time and money on treatments that won’t work. Contact us today for accurate diagnosis and effective fungal acne management that delivers real results.