Contact Dermatitis: Complete Clinical Guide for Diagnosis and Management
Contact dermatitis represents one of the most prevalent dermatological conditions encountered in clinical practice, affecting approximately 15-20% of the global population at some point during their lifetime. This inflammatory skin condition results from direct contact between the skin and specific substances that either irritate the skin directly or trigger an allergic immune response.
The clinical significance of contact dermatitis extends beyond mere skin irritation, often impacting patients’ quality of life, occupational capabilities, and psychological well-being. In Pakistan’s diverse industrial and cultural landscape, contact dermatitis presents unique diagnostic and therapeutic challenges, requiring comprehensive understanding of local allergens, occupational exposures, and traditional practices that may contribute to sensitization.
This comprehensive guide provides healthcare professionals with evidence-based information for accurate diagnosis, effective treatment protocols, and long-term management strategies for contact dermatitis in clinical practice.
Pathophysiology and Classification:
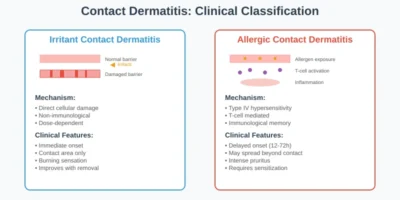
Contact dermatitis encompasses two distinct pathophysiological mechanisms, each requiring different diagnostic and therapeutic approaches. Understanding these fundamental differences is crucial for appropriate clinical management.
Irritant Contact Dermatitis:
Irritant contact dermatitis (ICD) represents a non-immunological inflammatory response resulting from direct cellular damage caused by exposure to irritating substances. This condition accounts for approximately 80% of all contact dermatitis cases in occupational settings.
Pathophysiological Mechanism: The development of ICD involves direct disruption of the skin barrier function through several mechanisms:
- Lipid extraction from the stratum corneum
- Protein denaturation in keratinocytes
- Direct cytotoxic effects on epidermal cells
- Disruption of intercellular junctions
- Activation of inflammatory cascades through cytokine release
Clinical Characteristics:
- Onset within minutes to hours of exposure
- Confined to areas of direct contact
- Dose-dependent response relationship
- No immunological memory component
- Immediate improvement upon removal of irritant
Common Irritants in Clinical Practice:
- Strong acids and alkalis
- Organic solvents
- Detergents and surfactants
- Friction and mechanical trauma
- Extreme temperatures
- Certain plants and biological materials
Allergic Contact Dermatitis:
Allergic contact dermatitis (ACD) represents a Type IV delayed-type hypersensitivity reaction mediated by T-lymphocytes. This condition requires prior sensitization and involves complex immunological processes.
Sensitization Phase: The development of ACD occurs through a two-phase process:
- Induction Phase: Initial contact with allergen leads to antigen processing by Langerhans cells, T-cell activation, and immunological memory formation
- Elicitation Phase: Subsequent exposure triggers rapid inflammatory response mediated by memory T-cells
Clinical Characteristics:
- Delayed onset (12-72 hours post-exposure)
- May extend beyond contact areas
- Dose-independent once sensitized
- Persistent immunological memory
- Progressive worsening with continued exposure
Immunological Cascade:
- Allergen penetration through compromised skin barrier
- Hapten-protein conjugate formation
- Langerhans cell antigen presentation
- T-helper cell activation and proliferation
- Cytokine-mediated inflammatory response
- Recruitment of inflammatory cells
Epidemiology and Risk Factors
Contact dermatitis demonstrates specific demographic patterns that influence clinical presentation and management strategies:
Age-Related Factors:
- Pediatric populations: Higher susceptibility due to immature barrier function
- Adult populations: Peak incidence in occupationally active age groups (20-40 years)
- Elderly patients: Increased risk due to compromised barrier function and polypharmacy
Gender Differences:
- Female predominance in cosmetic and jewelry allergies
- Male predominance in occupational contact dermatitis
- Hormonal influences on barrier function and immune responses
Genetic Predisposition:
- Family history of atopic conditions increases ACD risk
- Genetic polymorphisms affecting metabolic pathways
- Ethnic variations in sensitization patterns
Occupational Risk Factors
Occupational contact dermatitis represents a significant healthcare burden, with certain professions demonstrating elevated risk profiles:
High-Risk Occupations:
- Healthcare workers: Latex, disinfectants, medications
- Construction workers: Cement, adhesives, metals
- Hairdressers: PPD, formaldehyde, fragrances
- Food handlers: Proteins, preservatives, cleaning agents
- Textile workers: Dyes, formaldehyde resins, rubber chemicals
Workplace Assessment Considerations:
- Chemical exposure inventory
- Personal protective equipment adequacy
- Workplace hygiene protocols
- Environmental monitoring data
- Incident reporting systems
Clinical Assessment Protocol:
Comprehensive clinical evaluation forms the cornerstone of accurate contact dermatitis diagnosis, requiring systematic assessment of multiple factors.
History Taking:
- Detailed exposure history including timing and duration
- Occupational and recreational activities
- Personal care product usage patterns
- Previous episodes and treatment responses
- Family history of allergic conditions
- Current medications and topical applications
Physical Examination:
- Distribution pattern analysis
- Morphological characteristics assessment
- Acute vs. chronic lesion identification
- Secondary infection evaluation
- Extent and severity grading
Diagnostic Criteria: Established diagnostic criteria facilitate accurate clinical assessment:
- Compatible clinical presentation
- Relevant exposure history
- Appropriate anatomical distribution
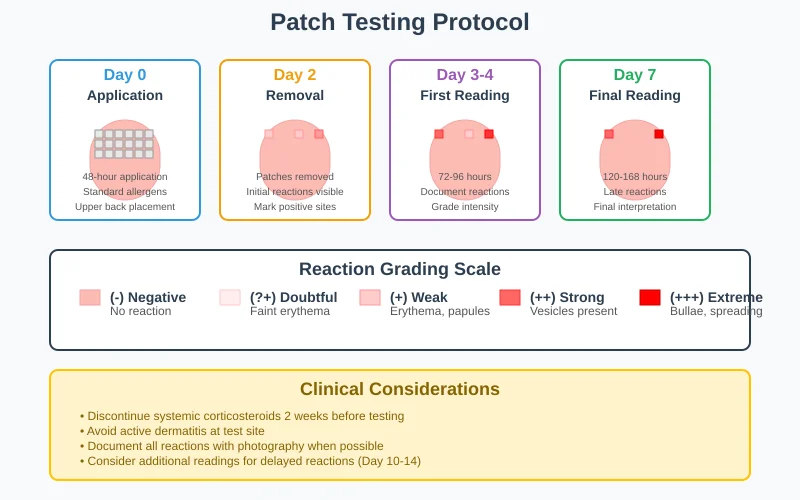
- Positive patch testing (for ACD)
- Improvement with allergen avoidance
Morphological Patterns
Acute Presentation:
- Erythema and edema
- Vesicle and bullae formation
- Weeping and crusting
- Intense pruritus or burning sensation
Chronic Presentation:
- Lichenification and hyperkeratosis
- Fissuring and scaling
- Hyperpigmentation or hypopigmentation
- Reduced inflammatory component
Distribution-Based Diagnosis:
- Linear patterns: Plant allergies, chemical splashes
- Geometric patterns: Cosmetic or topical medication reactions
- Localized patterns: Jewelry, clothing, or equipment contact
- Widespread patterns: Airborne allergens or systemic contact dermatitis
Differential Diagnosis
Accurate diagnosis requires exclusion of conditions with similar clinical presentations:
Atopic Dermatitis:
- Personal or family history of atopy
- Characteristic distribution patterns
- Chronicity and relapsing nature
- Elevated IgE levels
Seborrheic Dermatitis:
- Predilection for sebaceous areas
- Greasy scale characteristics
- Association with Malassezia overgrowth
Psoriasis:
- Well-demarcated plaques
- Silvery scale appearance
- Nail changes and arthritis
- Family history
Photodermatitis:
- Sun-exposed area distribution
- Seasonal variation patterns
- Phototesting confirmation
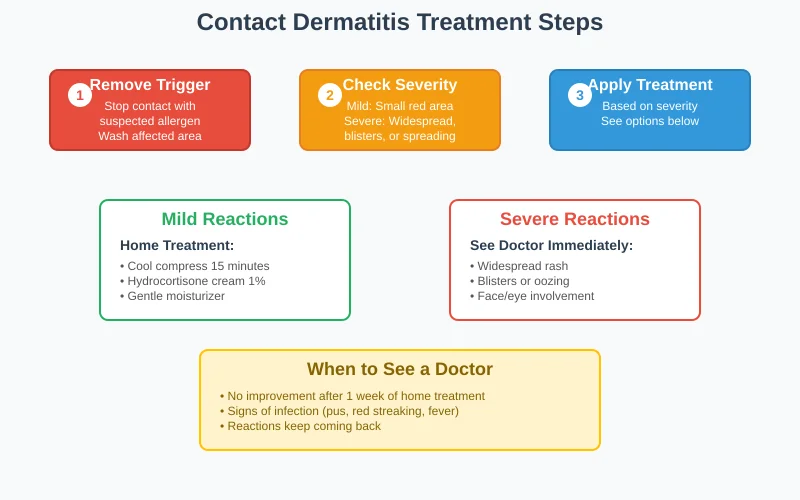
Treatment Protocols
Immediate Intervention:
- Allergen/irritant removal: Immediate cessation of suspected exposure
- Skin decontamination: Copious irrigation with water or saline
- Cool compresses: 15-20 minutes, 3-4 times daily for acute inflammation
- Barrier protection: Protective clothing or barriers for unavoidable exposures
Topical Therapy:
- Corticosteroids: First-line treatment for inflammatory component
- Mild potency: Hydrocortisone 1% for facial/intertriginous areas
- Moderate potency: Triamcinolone 0.1% for body areas
- High potency: Clobetasol 0.05% for severe, localized reactions
- Calcineurin inhibitors: Tacrolimus 0.1% or pimecrolimus 1% for maintenance
- Barrier repair agents: Ceramide-containing moisturizers for restoration
Systemic Therapy:
- Oral corticosteroids: Severe, widespread reactions
- Prednisone 1mg/kg/day (maximum 60mg) for 2-3 weeks
- Gradual tapering to prevent rebound reactions
- Antihistamines: Symptomatic relief of pruritus
- H1 antagonists: Cetirizine 10mg daily or loratadine 10mg daily
- Sedating antihistamines: Hydroxyzine 25-50mg at bedtime
Chronic Management Approaches
Long-term Care Strategies:
- Allergen avoidance: Primary prevention strategy
- Skin barrier optimization: Regular moisturizing protocols
- Occupational modifications: Workplace accommodation when necessary
- Patient education: Comprehensive allergen awareness programs
Maintenance Therapy:
- Topical immunomodulators: Long-term anti-inflammatory therapy
- Moisturizing regimens: Twice-daily application of emollients
- pH optimization: Slightly acidic cleansers and moisturizers
- Environmental modifications: Humidity control and allergen reduction
Refractory Cases Management
Advanced Treatment Options:
- Immunosuppressive therapy: Methotrexate, azathioprine, or cyclosporine
- Phototherapy: UVB or PUVA for chronic, widespread disease
- Biologic therapy: Dupilumab for severe, treatment-resistant cases
- Allergen immunotherapy: Investigational approaches for specific allergens
Prevention and Occupational Health
Workplace Interventions:
- Engineering controls: Ventilation systems, enclosed processes
- Administrative controls: Job rotation, training programs
- Personal protective equipment: Appropriate glove selection, protective clothing
- Surveillance programs: Regular health monitoring and early detection
Personal Care Modifications:
- Product selection: Hypoallergenic, fragrance-free alternatives
- Patch testing: Pre-exposure testing for suspected allergens
- Barrier methods: Protective gloves, clothing, or topical barriers
- Hygiene protocols: Proper hand washing and skin care routines
Secondary Prevention:
- Prompt treatment: Immediate management of initial symptoms
- Allergen identification: Comprehensive testing for sensitized individuals
- Workplace modifications: Job accommodation and environmental changes
- Education programs: Patient and family allergen awareness training
Tertiary Prevention:
- Secondary infection prevention: Appropriate antibiotic therapy when indicated
- Scarring minimization: Early aggressive treatment of severe reactions
- Psychological support: Counseling for quality of life impacts
- Disability assessment: Occupational capacity evaluation when necessary
Special Populations and Considerations
Pediatric Contact Dermatitis:
- Anatomical differences: Thinner stratum corneum, higher surface area to body weight ratio
- Behavioral factors: Increased hand-to-mouth contact, exploration behaviors
- Common allergens: Nickel (jewelry, clothing fasteners), fragrances (bubble baths), preservatives
Treatment Modifications:
- Lower potency topical corticosteroids
- Shorter treatment durations
- Enhanced barrier protection measures
- Family education and environmental modifications
Pregnancy and Contact Dermatitis
Safety Considerations:
- Topical therapy: Category B topical corticosteroids preferred
- Systemic therapy: Avoid systemic corticosteroids in first trimester when possible
- Allergen exposure: Increased vigilance for occupational and household exposures
- Hormonal influences: Possible changes in sensitization patterns
Elderly Population
Age-Related Factors:
- Barrier function decline: Increased susceptibility to irritants
- Polypharmacy effects: Multiple potential sensitizers
- Healing delays: Prolonged recovery periods
- Cognitive considerations: Compliance challenges with complex regimens
Factors Influencing Prognosis
Positive Prognostic Factors:
- Early diagnosis and appropriate treatment
- Successful allergen identification and avoidance
- Adequate occupational modifications
- Good patient compliance with treatment regimens
Negative Prognostic Factors:
- Delayed diagnosis or treatment
- Continued allergen exposure
- Multiple sensitizations
- Occupational limitations or restrictions
Monitoring Protocols:
- Regular follow-up: Assessment of disease control and treatment efficacy
- Repeat patch testing: When new sensitizations are suspected
- Occupational health surveillance: Ongoing workplace monitoring
- Complication screening: Early detection and management of secondary issues
Emerging Diagnostic Technologies
Advanced Testing Methods:
- Molecular allergology: Component-resolved diagnostics
- In vitro testing: Lymphocyte transformation tests, cytokine release assays
- Imaging techniques: Confocal microscopy, optical coherence tomography
- Biomarker development: Serum and tissue markers for disease activity
Novel Therapeutic Approaches
Innovative Treatments:
- Targeted immunotherapy: Specific allergen desensitization protocols
- Topical immunomodulators: Next-generation calcineurin inhibitors
- Biologic therapy: Targeted cytokine inhibition
- Regenerative medicine: Stem cell therapy and tissue engineering applications
Conclusion:
Contact dermatitis represents a complex dermatological condition requiring comprehensive clinical expertise for accurate diagnosis and effective management. The distinction between irritant and allergic mechanisms, combined with thorough allergen identification through appropriate testing, forms the foundation for successful treatment outcomes.
Healthcare providers must maintain awareness of evolving allergen exposures, occupational hazards, and cultural practices that may contribute to sensitization patterns. The integration of evidence-based treatment protocols with individualized patient care strategies ensures optimal therapeutic outcomes while minimizing long-term complications.
Continued research into pathophysiological mechanisms, diagnostic innovations, and therapeutic advances will further enhance our ability to provide effective care for patients with contact dermatitis, ultimately improving quality of life and reducing the substantial healthcare burden associated with this prevalent condition.
For comprehensive contact dermatitis evaluation, including professional patch testing and personalized treatment protocols, consult with the experienced dermatologists at Derma & Dental Clinic. Our team provides evidence-based care tailored to individual patient needs and Pakistan’s unique environmental and occupational challenges.