Hyperhidrosis: Understanding and Treating Excessive Sweating
Excessive sweating, medically known as hyperhidrosis, affects millions of people worldwide, causing significant physical discomfort and emotional distress that can severely impact daily activities, professional performance, and social interactions. While sweating is a normal bodily function essential for temperature regulation, hyperhidrosis involves sweating that far exceeds the body’s physiological needs, often occurring even in cool environments or during rest.
In Pakistan’s hot and humid climate, where temperatures frequently exceed 40°C and humidity levels can reach 80%, distinguishing between normal heat-related sweating and pathological hyperhidrosis becomes particularly challenging. However, true hyperhidrosis persists regardless of environmental conditions and can significantly affect quality of life, making professional medical evaluation and treatment essential.
Understanding the underlying mechanisms, accurate diagnosis, and comprehensive treatment options available for hyperhidrosis enables patients to regain control over their symptoms and improve their overall quality of life through evidence-based medical interventions.
Understanding the Physiology of Sweating
Normal sweating serves as the body’s primary cooling mechanism, regulated by the sympathetic nervous system through approximately 2-4 million sweat glands distributed across the body. The two main types of sweat glands each serve different functions in maintaining body temperature and responding to various stimuli.
Eccrine Glands: These are the primary glands responsible for thermoregulation, found in highest concentrations on the palms, soles, forehead, and underarms. Eccrine glands produce a clear, odorless fluid composed primarily of water, sodium chloride, and trace amounts of other electrolytes. These glands respond directly to thermal stimuli and emotional stress through sympathetic nervous system activation.
Apocrine Glands: Located primarily in the axillary (underarm) and groin regions, apocrine glands produce a thicker, protein-rich secretion that becomes odorous when metabolized by skin bacteria. These glands typically become active during puberty and respond more to emotional and hormonal stimuli than thermal stress.
The sweating response involves complex neurological pathways beginning in the hypothalamus, which serves as the body’s thermostat. When core body temperature rises or emotional stress occurs, the hypothalamus signals the sympathetic nervous system to activate sweat glands through acetylcholine release, triggering fluid production and evaporative cooling.
Types and Classification of Hyperhidrosis
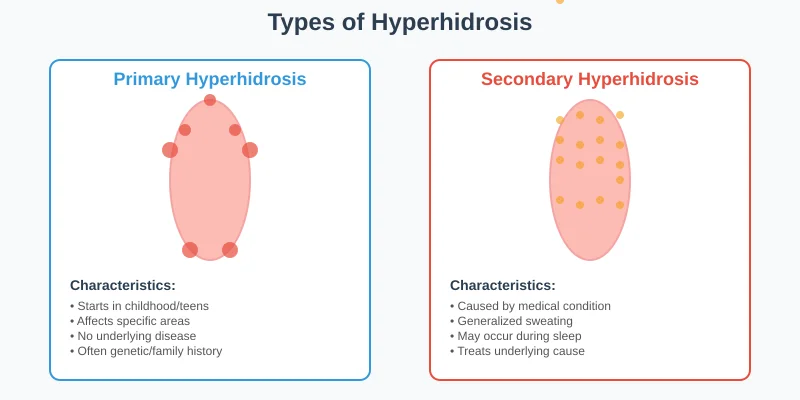
Primary Hyperhidrosis (Essential Hyperhidrosis)
Primary hyperhidrosis represents the most common form of excessive sweating, affecting approximately 2-3% of the global population. This condition appears to have a strong genetic component, with family history present in 30-50% of cases, suggesting inherited abnormalities in sympathetic nervous system function.
Characteristics of Primary Hyperhidrosis:
- Onset typically during childhood or adolescence
- Bilateral and symmetrical distribution patterns
- Focal involvement of specific body areas
- Absence of sweating during sleep
- No underlying medical condition identified
- Often triggered or worsened by emotional stress
Common Locations:
- Palmar hyperhidrosis: Excessive hand sweating affecting grip and fine motor activities
- Axillary hyperhidrosis: Underarm sweating causing clothing stains and social embarrassment
- Plantar hyperhidrosis: Foot sweating leading to footwear problems and fungal infections
- Craniofacial hyperhidrosis: Head and face sweating affecting professional and social interactions
Secondary Hyperhidrosis
Secondary hyperhidrosis results from underlying medical conditions, medications, or hormonal changes that affect the normal sweating mechanism. This form typically presents with generalized sweating patterns and may occur during sleep, helping distinguish it from primary hyperhidrosis.
Medical Conditions Causing Secondary Hyperhidrosis:
- Endocrine disorders: Hyperthyroidism, diabetes mellitus, menopause, pheochromocytoma
- Neurological conditions: Parkinson’s disease, spinal cord injuries, stroke, neuropathies
- Infections: Tuberculosis, malaria, endocarditis, HIV-related conditions
- Malignancies: Lymphomas, leukemias, solid tumors with paraneoplastic syndromes
- Cardiovascular conditions: Heart failure, shock, cardiovascular collapse
- Psychiatric disorders: Anxiety disorders, panic attacks, depression with anxiety
Medications Associated with Hyperhidrosis:
- Antidepressants (particularly SSRIs and tricyclics)
- Anxiolytics and psychiatric medications
- Pain medications including opioids
- Blood pressure medications
- Hormonal therapies and oral contraceptives
- Antibiotics and antimalarial drugs
Causes and Contributing Factors
Genetic and Hereditary Influences
Research indicates that primary hyperhidrosis has a strong hereditary component, with studies showing familial clustering in 30-65% of cases. The exact genetic mechanisms remain under investigation, but evidence suggests autosomal dominant inheritance patterns with variable penetrance and expression.
Recent genetic studies have identified potential chromosomal loci associated with hyperhidrosis susceptibility, particularly involving genes that regulate sympathetic nervous system function and neurotransmitter metabolism. However, the condition likely involves multiple genetic factors rather than a single gene defect.
Family History Patterns:
- Higher prevalence in first-degree relatives
- Earlier onset in subsequent generations (anticipation phenomenon)
- Similar anatomical distribution patterns within families
- Varying severity levels among affected family members
Environmental and Lifestyle Factors
While primary hyperhidrosis has genetic underpinnings, environmental factors can significantly influence symptom severity and frequency. Pakistan’s climate presents unique challenges that can exacerbate sweating in susceptible individuals.
Climate-Related Factors:
- High ambient temperatures increasing baseline sweating
- Elevated humidity levels reducing evaporative cooling efficiency
- Sudden temperature changes between air-conditioned and outdoor environments
- Seasonal variations affecting symptom severity
- Occupational heat exposure in various industries
Lifestyle Influences:
- Diet: Spicy foods, caffeine, and alcohol can trigger sweating episodes
- Stress levels: Work pressure, social anxiety, and emotional stress
- Physical activity: Exercise intensity and duration
- Clothing choices: Synthetic fabrics and tight-fitting garments
- Sleep patterns: Irregular sleep affecting nervous system regulation
Psychological and Emotional Components
The relationship between hyperhidrosis and psychological factors is complex and bidirectional. While emotional stress can trigger sweating episodes, the social embarrassment and functional limitations caused by excessive sweating can lead to anxiety, depression, and social withdrawal.
Psychological Triggers:
- Social anxiety and fear of embarrassment
- Performance anxiety in professional or academic settings
- General anxiety disorders and panic attacks
- Depression with associated autonomic dysfunction
- Post-traumatic stress responses
Secondary Psychological Effects:
- Social isolation and withdrawal from activities
- Reduced self-confidence and self-esteem
- Depression related to functional limitations
- Anxiety about sweating episodes creating a vicious cycle
Diagnostic Evaluation and Assessment
Clinical History and Physical Examination
Comprehensive evaluation begins with detailed history taking to distinguish primary from secondary hyperhidrosis and assess the impact on daily functioning. The diagnostic process helps determine appropriate treatment strategies and rule out underlying medical conditions.
Essential History Components:
- Age of onset and progression patterns
- Anatomical distribution and severity assessment
- Triggering factors and temporal patterns
- Family history of hyperhidrosis or related conditions
- Current medications and medical history
- Impact on occupational, social, and personal activities
- Previous treatments attempted and their effectiveness
Physical Examination Elements:
- Assessment of sweating patterns and distribution
- Evaluation for signs of underlying medical conditions
- Neurological examination for autonomic dysfunction
- Thyroid examination and vital sign assessment
- Skin examination for secondary complications
Objective Measurement Techniques
Gravimetric Testing: This quantitative method involves weighing filter papers before and after placement on affected areas for a standardized time period. Normal sweating produces less than 20mg in 5 minutes, while hyperhidrosis typically exceeds 50mg in the same timeframe.
Starch-Iodine Test (Minor’s Test): An iodine solution is applied to the affected area, followed by starch powder. Active sweat glands produce a dark blue-black color change, creating a visual map of sweating patterns and intensity. This test helps evaluate treatment responses and plan intervention strategies.
Thermoregulatory Sweat Test: Used primarily in research settings, this comprehensive test evaluates the body’s entire sweating response to controlled heat exposure, helping distinguish neurological causes and assess overall autonomic function.
Laboratory and Specialized Testing
When secondary hyperhidrosis is suspected, appropriate laboratory investigations help identify underlying conditions requiring specific treatment.
Standard Laboratory Tests:
- Complete blood count and comprehensive metabolic panel
- Thyroid function tests (TSH, T3, T4)
- Fasting glucose and hemoglobin A1c
- Urinalysis and kidney function assessment
- Inflammatory markers (ESR, CRP) if infection suspected
Specialized Testing When Indicated:
- 24-hour urine catecholamines for pheochromocytoma
- Tuberculin skin test or interferon-gamma release assays
- Chest X-ray and imaging studies for malignancy screening
- Cardiac evaluation for cardiovascular causes
- Neurological testing for autonomic neuropathies
Comprehensive Treatment Approaches
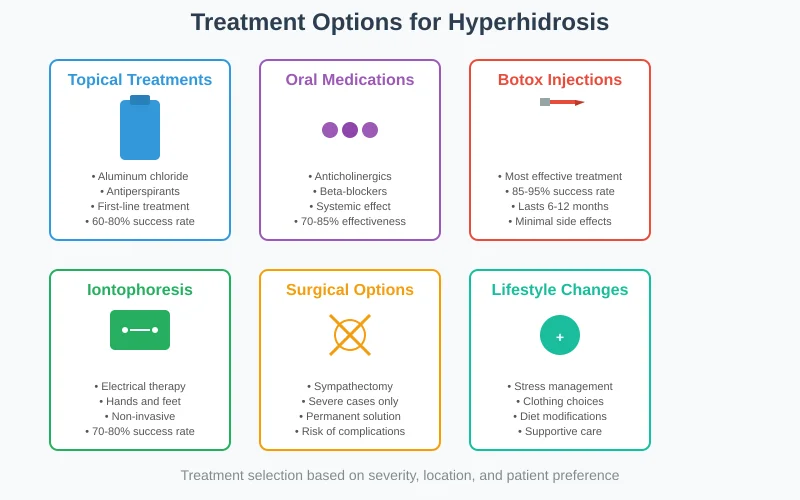
Topical Therapies and Antiperspirants
Aluminum-Based Antiperspirants: High-concentration aluminum chloride (10-25%) or aluminum chloride hexahydrate (6-20%) formulations represent first-line treatment for mild to moderate hyperhidrosis. These compounds work by forming plugs in sweat ducts, temporarily blocking perspiration.
Application Protocols:
- Apply to completely dry skin before bedtime
- Wash off in the morning to prevent irritation
- Use consistently for 4-6 weeks to assess effectiveness
- Start with lower concentrations to minimize skin irritation
- Gradually increase strength if needed and tolerated
Effectiveness and Considerations:
- Success rates of 60-80% for axillary hyperhidrosis
- Less effective for palmar and plantar hyperhidrosis
- Common side effects include skin irritation and contact dermatitis
- May cause clothing stains and fabric damage
- Requires consistent application for maintained effectiveness
Topical Anticholinergics: Glycopyrrolate gel (2-4%) offers an alternative for patients who cannot tolerate aluminum-based products. This medication blocks acetylcholine receptors, reducing sweat gland stimulation.
Advantages:
- Effective for facial hyperhidrosis where aluminum compounds may be too irritating
- Less likely to cause contact dermatitis
- Can be used during daytime hours
- Suitable for sensitive skin areas
Limitations:
- Requires prescription and may be more expensive
- Potential systemic absorption causing dry mouth or other anticholinergic effects
- May require compounding pharmacy preparation
- Limited long-term safety data
Oral Medications
Anticholinergic Medications: Systemic anticholinergic drugs like glycopyrrolate (1-2mg twice daily) or oxybutynin (2.5-5mg twice daily) can be effective for generalized hyperhidrosis or when topical treatments fail.
Mechanism and Effectiveness:
- Block acetylcholine receptors throughout the body
- Reduce sweating by 50-80% in responsive patients
- Particularly effective for generalized or craniofacial hyperhidrosis
- Results typically seen within 2-4 weeks of consistent use
Side Effects and Monitoring:
- Dry mouth, dry eyes, and constipation (most common)
- Potential cognitive effects, especially in elderly patients
- Heat intolerance due to reduced sweating capacity
- Urinary retention in susceptible individuals
- Regular monitoring required for long-term use
Beta-Blockers: For patients with anxiety-related sweating or performance-related hyperhidrosis, beta-blockers like propranolol (10-40mg as needed) can be helpful.
Indications:
- Situational sweating related to anxiety or stress
- Performance anxiety causing excessive sweating
- Combination with other treatments for comprehensive management
- Patients with concurrent cardiovascular conditions
Advanced Treatment Modalities
Botulinum Toxin Injections: Botulinum toxin (Botox, Dysport) injections represent one of the most effective treatments for localized hyperhidrosis, providing temporary but significant sweat reduction.
Mechanism of Action:
- Blocks acetylcholine release at neuromuscular junctions
- Prevents nerve stimulation of sweat glands
- Localized effect without systemic complications
- Reversible with effects lasting 4-12 months
Treatment Protocols:
- Axillary hyperhidrosis: 50-100 units per axilla using intradermal injections
- Palmar hyperhidrosis: 100-200 units per palm with nerve blocks for comfort
- Plantar hyperhidrosis: 100-300 units per foot depending on surface area
- Facial hyperhidrosis: Lower doses (10-50 units) with careful placement
Effectiveness and Outcomes:
- 80-95% reduction in sweating for axillary hyperhidrosis
- 85-95% patient satisfaction rates
- Duration of effect typically 6-12 months
- Repeat treatments maintain effectiveness
- Minimal systemic side effects when properly administered
Side Effects and Considerations:
- Temporary injection site discomfort and bruising
- Potential weakness in nearby muscles (especially hands and feet)
- Cost considerations for repeated treatments
- Need for experienced injector to minimize complications
- Insurance coverage varies but increasingly available
Iontophoresis: This non-invasive treatment uses low-level electrical current passed through water to temporarily disable sweat glands, particularly effective for palmar and plantar hyperhidrosis.
Treatment Protocol:
- Hands or feet immersed in water with electrical current
- Sessions last 20-40 minutes, typically 3 times weekly initially
- Maintenance treatments 1-2 times weekly after improvement
- Home devices available for long-term management
Effectiveness:
- 70-80% success rate for palmar and plantar hyperhidrosis
- Less effective for axillary or facial hyperhidrosis
- Results typically seen after 6-10 treatment sessions
- Maintenance therapy required to sustain benefits
Advantages and Limitations:
- Non-invasive with minimal side effects
- Can be performed at home with proper equipment
- No systemic medications required
- Time-intensive treatment schedule
- Initial equipment cost and ongoing maintenance
Surgical Interventions
Endoscopic Thoracic Sympathectomy (ETS): For severe, treatment-resistant palmar hyperhidrosis, surgical interruption of sympathetic nerve pathways can provide permanent relief but carries significant risks.
Surgical Procedure:
- Minimally invasive thoracoscopic approach
- Interruption or removal of sympathetic ganglia (T2-T4)
- Usually performed bilaterally in single procedure
- General anesthesia required with overnight observation
Effectiveness:
- Near 100% success rate for palmar hyperhidrosis
- Immediate and permanent results
- High patient satisfaction when successful
- Also effective for facial and axillary hyperhidrosis
Complications and Considerations:
- Compensatory hyperhidrosis in 50-90% of patients (trunk, legs, feet)
- Gustatory sweating when eating certain foods
- Potential sexual dysfunction in males
- Irreversible procedure with permanent effects
- Reserved for severe cases unresponsive to other treatments
Local Surgical Procedures: For axillary hyperhidrosis, local surgical removal of sweat glands or tissue may be considered in select cases.
Surgical Options:
- Curettage: Scraping removal of sweat glands
- Liposuction: Suction removal of glandular tissue
- Excision: Direct surgical removal of affected tissue
Considerations:
- Limited to axillary region
- Risk of scarring and skin changes
- Potential infection and healing complications
- Less invasive than sympathectomy but more than medical treatments
Treatment Selection and Individualized Care
Patient Assessment and Treatment Planning
Effective hyperhidrosis management requires individualized treatment plans based on symptom severity, anatomical location, patient preferences, and response to previous therapies.
Severity Classification:
- Mild: Noticeable sweating but minimal impact on daily activities
- Moderate: Sweating interferes with some activities and causes social concern
- Severe: Sweating significantly impairs daily functioning and quality of life
Treatment Algorithm:
- First-line: Topical antiperspirants for localized mild-moderate hyperhidrosis
- Second-line: Oral anticholinergics or iontophoresis for widespread or resistant cases
- Third-line: Botulinum toxin injections for localized severe hyperhidrosis
- Fourth-line: Surgical consultation for treatment-resistant severe cases
Combination Therapy Approaches
Many patients benefit from combining multiple treatment modalities to achieve optimal symptom control and maintain long-term effectiveness.
Effective Combinations:
- Topical antiperspirants with oral anticholinergics for comprehensive coverage
- Botulinum toxin injections with maintenance topical therapy
- Iontophoresis with topical treatments for enhanced effectiveness
- Stress management techniques with medical therapies
Maintenance Strategies:
- Regular follow-up to assess treatment effectiveness
- Adjustment of therapies based on seasonal variations
- Patient education about trigger avoidance
- Psychological support for coping strategies
Living with Hyperhidrosis: Practical Management
Lifestyle Modifications and Coping Strategies
Clothing and Fabric Choices:
- Natural fiber clothing (cotton, linen) for better moisture absorption
- Loose-fitting garments to improve air circulation
- Layered clothing to manage temperature variations
- Dark or patterned fabrics to camouflage potential stains
- Moisture-wicking athletic wear for exercise activities
Personal Hygiene and Skin Care:
- Regular bathing with antibacterial soaps to prevent odor
- Complete drying of skin before applying antiperspirants
- Foot hygiene including antifungal powders for plantar hyperhidrosis
- Regular changing of socks and undergarments
- Skin barrier protection in areas prone to irritation
Environmental Modifications:
- Air conditioning and fan use for temperature control
- Cooling strategies during hot weather exposure
- Stress reduction techniques including meditation and relaxation
- Avoiding known triggers such as spicy foods or caffeine
- Planning activities during cooler parts of the day
Psychological Support and Quality of Life
Counseling and Therapy:
- Cognitive-behavioral therapy for anxiety and stress management
- Support groups for patients with hyperhidrosis
- Social skills training for confidence building
- Stress management techniques and relaxation training
Professional and Social Considerations:
- Workplace accommodations when possible
- Career guidance considering physical limitations
- Relationship counseling for interpersonal impacts
- Educational support for children and adolescents with hyperhidrosis
Prognosis and Long-term Management
Expected Outcomes with Treatment
Success Rates by Treatment Type:
- Topical antiperspirants: 60-80% improvement in appropriate candidates
- Oral anticholinergics: 70-85% reduction in sweating with good tolerance
- Botulinum toxin: 85-95% patient satisfaction with proper administration
- Iontophoresis: 70-80% success for palmar and plantar hyperhidrosis
- Surgical procedures: Near 100% success but with potential complications
Factors Affecting Treatment Success:
- Early intervention generally produces better outcomes
- Patient compliance with prescribed therapies
- Appropriate treatment selection based on hyperhidrosis type and severity
- Management of underlying conditions in secondary hyperhidrosis
- Realistic expectations and ongoing medical support
Long-term Management Strategies
Maintenance Therapy:
- Regular assessment of treatment effectiveness
- Adjustment of therapies based on life changes and seasonal variations
- Monitoring for side effects and complications
- Integration of new treatment options as they become available
Quality of Life Monitoring:
- Regular assessment of functional impact and social functioning
- Psychological support as needed throughout treatment course
- Career and educational guidance for young patients
- Family counseling and support system development
Prevention and Risk Reduction
Primary Prevention Strategies
While primary hyperhidrosis cannot be prevented due to its genetic nature, several strategies can help minimize symptom severity and frequency.
Trigger Avoidance:
- Identifying and avoiding personal sweating triggers
- Stress management and anxiety reduction techniques
- Dietary modifications to avoid sweating-inducing foods
- Environmental control when possible
- Regular exercise to improve overall autonomic function
Early Intervention:
- Prompt recognition and treatment of symptoms
- Family screening for early identification in at-risk individuals
- Education about condition and available treatments
- Prevention of secondary complications such as skin infections
Secondary Prevention
Complication Prevention:
- Skin care routines to prevent irritation and infection
- Foot care to prevent fungal infections in plantar hyperhidrosis
- Psychological support to prevent social withdrawal and depression
- Regular medical monitoring for treatment effectiveness and side effects
Conclusion
Hyperhidrosis represents a challenging medical condition that significantly impacts quality of life, but effective treatments are available for most patients. Understanding the distinction between primary and secondary hyperhidrosis, accurate diagnosis, and comprehensive treatment planning are essential for optimal outcomes.
Key principles for successful hyperhidrosis management:
- Comprehensive evaluation: Distinguish primary from secondary causes and assess severity
- Individualized treatment: Tailor therapy based on location, severity, and patient factors
- Stepwise approach: Begin with conservative treatments and advance based on response
- Combination strategies: Use multiple modalities for optimal symptom control
- Long-term planning: Develop maintenance strategies and provide ongoing support
- Quality of life focus: Address both physical symptoms and psychosocial impacts
Modern treatment options offer hope for patients with hyperhidrosis, enabling them to regain control over their symptoms and improve their overall quality of life. At Derma & Dental Clinic, our experienced dermatologists provide comprehensive evaluation and individualized treatment plans using the latest evidence-based therapies.
Don’t let excessive sweating control your life. Contact us today for expert evaluation and personalized treatment strategies that can help you achieve lasting relief from hyperhidrosis and restore your confidence in professional and social situations.
