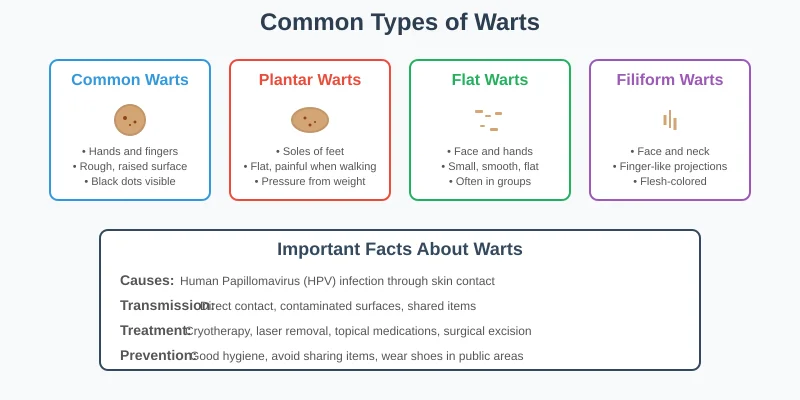
Warts: Types, Causes, and Modern Removal Methods
Warts are among the most common skin conditions encountered in dermatological practice, affecting millions of people worldwide regardless of age, gender, or socioeconomic status. These benign but often troublesome growths can appear anywhere on the body, causing physical discomfort, cosmetic concerns, and significant psychological distress, particularly when they occur in visible areas or interfere with daily activities.
Despite being non-cancerous, warts present unique challenges due to their viral nature, tendency to spread, and frequent recurrence even after treatment. Many people attempt self-treatment with over-the-counter remedies or home remedies, often leading to complications, scarring, or worsening of the condition. Understanding the viral causes, different types, and evidence-based treatment options is essential for effective management and prevention of complications.
In Pakistan’s diverse climate and social environment, warts spread easily in communal areas like mosques, gyms, swimming pools, and schools. Professional dermatological evaluation and treatment ensure safe, effective removal while minimizing the risk of spread to others and preventing long-term complications that can result from improper treatment attempts.
Understanding the Viral Nature of Warts
Warts are caused by human papillomavirus (HPV), a large family of DNA viruses with over 100 different types, each with specific preferences for certain body areas and manifestations. The virus infects the top layer of skin through tiny cuts or breaks, causing rapid multiplication of skin cells that results in the characteristic rough, raised appearance of warts.
How HPV Infection Occurs:
The virus enters through microscopic breaks in the skin barrier, often so small they’re invisible to the naked eye. Once inside, HPV infects the basal cells of the epidermis, disrupting normal cellular regulation and causing excessive keratinocyte proliferation. The infected cells produce viral proteins that interfere with normal cell cycle control, leading to the characteristic thickened, hyperkeratotic appearance of warts.
Viral Transmission Mechanisms:
HPV spreads through direct skin-to-skin contact with infected individuals or contaminated surfaces. The virus can survive on surfaces for extended periods, making transmission possible through shared items like towels, shoes, or walking barefoot in communal areas. Factors that increase transmission risk include damaged skin barriers, compromised immune function, and prolonged exposure to moist environments where the virus thrives.
Immune System Response:
The body’s immune response to HPV infection varies significantly among individuals, explaining why some people develop multiple warts while others remain unaffected despite exposure. Cell-mediated immunity plays a crucial role in controlling HPV infection, which is why immunocompromised individuals often experience more severe, persistent, or widespread wart infections.
Common Warts (Verruca Vulgaris):
Common warts represent the most frequently encountered type, typically caused by HPV types 1, 2, 4, and 7. These warts have a distinctive appearance that makes them relatively easy to identify, though they can vary in size and number depending on individual factors and duration of infection.
Clinical Characteristics: Common warts appear as firm, raised growths with a rough, cauliflower-like surface texture. They typically range from 1-10mm in diameter but can grow larger if left untreated. The surface often shows characteristic black dots, which are thrombosed capillaries, not “seeds” as commonly believed. These warts have well-defined borders and a grayish-brown color.
Typical Locations:
- Hands and fingers (most common sites)
- Around fingernails and cuticles
- Knees and elbows
- Face in children
- Any area prone to minor trauma or cuts
Behavior and Progression: Common warts tend to grow slowly over months to years. They may remain single or multiply through local spread or auto-inoculation. In children, these warts often resolve spontaneously within 2-3 years as the immune system matures, while adult cases may persist longer without treatment.
Plantar Warts (Verruca Plantaris):
Plantar warts occur on the soles of feet and are caused primarily by HPV types 1, 2, 4, and 63. The pressure from walking causes these warts to grow inward rather than outward, making them particularly painful and challenging to treat.
Distinctive Features: Unlike other warts, plantar warts appear flat due to pressure from walking. They often have a hard, callused surface with black pinpoint dots representing thrombosed capillaries. The surrounding skin may be raised, and the wart itself may be surrounded by a callus ring. Pain occurs when pressure is applied directly to the wart.
Types of Plantar Warts:
- Solitary warts: Single, larger lesions that can be quite painful
- Mosaic warts: Multiple small warts clustered together, less painful but more extensive
Impact on Daily Life: Plantar warts can significantly affect mobility and quality of life. The pain may cause altered gait patterns, leading to secondary problems in ankles, knees, or hips. Athletic activities become difficult, and choosing appropriate footwear becomes challenging.
Flat Warts (Verruca Plana):
Flat warts, caused primarily by HPV types 3 and 10, are smaller and smoother than common warts. They appear as slightly raised, flat-topped lesions that can be pink, brown, or yellow in color, making them sometimes difficult to notice initially.
Clinical Appearance: These warts are typically 1-4mm in diameter with a smooth, flat surface. They often appear in groups of 20-100 lesions and have a characteristic linear arrangement when they spread through scratching or shaving trauma (Koebner phenomenon).
Common Locations:
- Face (especially in children)
- Forehead and temples
- Hands and arms
- Legs (particularly in women who shave)
- Back of hands in adults
Special Considerations: Flat warts are particularly concerning when they occur on the face due to cosmetic implications. They spread easily through shaving or scratching, often appearing in linear patterns. Treatment requires careful consideration to avoid scarring in cosmetically sensitive areas.
Filiform Warts:
These distinctive warts have a finger-like, thread-like appearance and are caused by specific HPV types including 1, 2, 4, 27, and 29. They typically occur on the face, neck, and eyelids, making them particularly noticeable and cosmetically concerning.
Unique Characteristics: Filiform warts appear as narrow, elongated growths that protrude from the skin surface. They’re usually flesh-colored or slightly darker and can grow quickly. Unlike other wart types, they don’t have the rough, hyperkeratotic surface typical of common warts.
Treatment Considerations: Due to their location on the face and neck, filiform warts require careful treatment approaches that minimize scarring risk. Their projecting nature makes them prone to trauma and bleeding, which can facilitate spread to surrounding areas.
Genital Warts (Condyloma Acuminatum):
Genital warts are caused by specific HPV types, most commonly 6 and 11, and are transmitted through sexual contact. While generally benign, they require specialized medical management due to their location, transmission implications, and potential association with oncogenic HPV types.
Clinical Presentation: Genital warts appear as soft, flesh-colored or slightly darker growths that can be flat or raised. They may occur singly or in clusters, sometimes forming large, cauliflower-like masses. The texture is typically softer and more moist than other wart types due to the anatomical location.
Location-Specific Considerations:
- External genital areas in both men and women
- Anal area and perianal region
- Internal genital areas (requiring specialized examination)
- Oral cavity in cases of oral transmission
Medical and Social Implications: Genital warts require comprehensive sexually transmitted infection evaluation, partner notification and treatment, and long-term monitoring for potential complications. They can cause significant psychological distress and relationship concerns.
Causes and Risk Factors
Viral Transmission Pathways:
Understanding how HPV spreads helps in both treatment and prevention strategies. The virus requires direct contact with infected skin or contaminated surfaces, but several factors influence transmission likelihood and infection establishment.
Direct Contact Transmission:
- Skin-to-skin contact with infected individuals
- Sexual transmission for genital wart types
- Mother-to-child transmission during delivery (rare)
- Auto-inoculation through scratching or picking existing warts
Indirect Transmission Sources:
- Contaminated surfaces in public areas (pools, showers, locker rooms)
- Shared personal items (towels, razors, nail files)
- Walking barefoot in communal areas
- Contaminated medical or beauty equipment
Individual Risk Factors:
Immune System Status: People with compromised immune systems face significantly higher risk for wart development and more severe, persistent infections. This includes individuals with HIV/AIDS, organ transplant recipients, those on immunosuppressive medications, and people with certain genetic immunodeficiencies.
Age-Related Susceptibility: Children and teenagers show higher susceptibility to common warts due to developing immune systems and increased exposure opportunities in school settings. Adults may be more susceptible to certain types based on lifestyle factors and occupational exposures.
Skin Barrier Integrity: Damaged skin provides easier viral entry points. Factors that compromise skin integrity include:
- Occupational exposures (healthcare workers, food handlers)
- Chronic skin conditions (eczema, dry skin)
- Habitual nail-biting or cuticle picking
- Frequent hand washing or water exposure
- Minor cuts and abrasions
Environmental and Occupational Factors: Certain occupations and activities increase wart risk through increased viral exposure or skin trauma:
- Healthcare workers (especially those handling contaminated materials)
- Food service workers (frequent hand washing and cuts)
- Athletes using communal facilities
- Swimming instructors and lifeguards
- People working in humid environments
Clinical Diagnosis:
Most warts can be diagnosed through careful visual examination by experienced dermatologists. The characteristic appearance, location, and patient history usually provide sufficient information for accurate diagnosis.
Diagnostic Features:
- Surface texture and appearance
- Location and distribution patterns
- Response to pressure or manipulation
- Associated symptoms (pain, itching)
- Progression over time
Differential Diagnosis Considerations: Several conditions can mimic warts, making professional evaluation important:
- Seborrheic keratoses
- Corns and calluses
- Molluscum contagiosum
- Skin cancers (rare but important to exclude)
- Foreign body reactions
Advanced Diagnostic Techniques:
Dermoscopy: Dermatoscopic examination can help confirm wart diagnosis by revealing characteristic features like thrombosed capillaries (black dots) and papillary surface patterns that distinguish warts from other skin lesions.
HPV Typing: While not routinely necessary for common warts, HPV typing may be valuable in certain situations:
- Recurrent or treatment-resistant genital warts
- Unusual clinical presentations
- Research or epidemiological studies
- Risk assessment for oncogenic potential
Histopathological Examination: Biopsy is rarely needed for typical warts but may be considered when:
- Diagnosis is uncertain
- Lesions fail to respond to appropriate treatment
- Atypical features suggest other conditions
- Malignant transformation is suspected
Comprehensive Treatment Strategies
First-Line Treatment Options
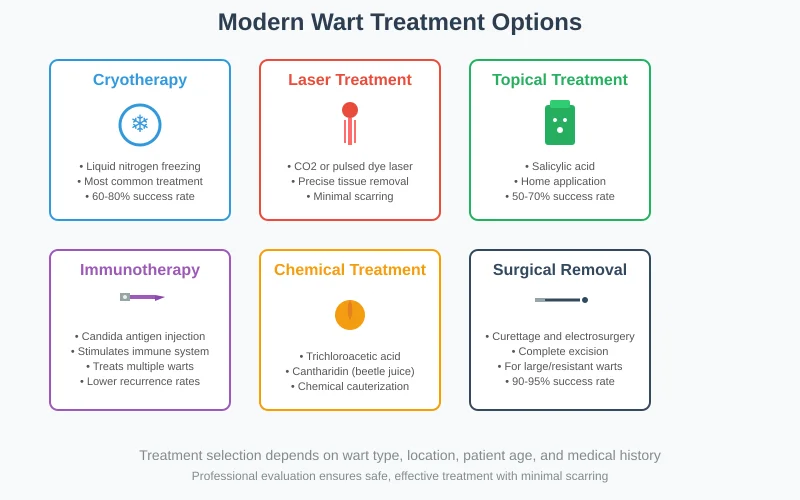
Cryotherapy (Liquid Nitrogen) Cryotherapy remains one of the most widely used and effective treatments for various wart types. This procedure involves applying liquid nitrogen at -196°C to freeze and destroy infected tissue.
Mechanism of Action: The extreme cold causes cellular destruction through ice crystal formation, disrupting cell membranes and organelles. The subsequent inflammatory response may also help stimulate immune recognition of HPV-infected cells.
Treatment Protocol:
- Application for 10-30 seconds depending on wart size and location
- Repeat treatments every 2-3 weeks
- Usually requires 2-6 sessions for complete resolution
- Immediate whitening of tissue indicates adequate freezing
Effectiveness and Considerations:
- Success rates of 60-80% for common and plantar warts
- Less effective for flat warts and facial lesions
- Pain during and after treatment is common
- Risk of hypopigmentation, especially in darker skin types
- May cause blistering and temporary disability
Topical Treatments:
Salicylic Acid (15-40%): Available in various formulations including solutions, gels, and plasters, salicylic acid works by causing keratolysis and removing infected tissue layers.
Application Protocol:
- Soak affected area in warm water for 5-10 minutes
- File or pumice stone to remove softened tissue
- Apply salicylic acid preparation
- Cover with adhesive bandage
- Repeat daily for weeks to months
Advantages:
- Cost-effective and readily available
- Can be applied at home
- Minimal side effects when used properly
- Suitable for maintenance therapy
Limitations:
- Requires consistent daily application
- Success rates lower than office-based procedures
- May cause skin irritation or burns if misused
- Not suitable for facial or genital warts
Advanced Treatment Modalities:
Laser Therapy:
CO2 Laser: Carbon dioxide laser provides precise tissue vaporization with excellent hemostasis, making it particularly useful for large or resistant warts.
Advantages:
- Precise control over tissue removal
- Excellent hemostasis reduces bleeding
- Can treat multiple lesions in single session
- Good cosmetic outcomes when performed properly
Considerations:
- Requires local anesthesia
- Potential for scarring if overly aggressive
- Risk of viral transmission through laser plume
- More expensive than conventional treatments
Pulsed Dye Laser: This laser specifically targets blood vessels within warts, causing selective destruction while preserving surrounding tissue.
Mechanism: The 585nm wavelength is absorbed by hemoglobin in capillaries within the wart, causing thermal damage and subsequent tissue death.
Benefits:
- Less pain than CO2 laser
- Lower scarring risk
- Can be effective for resistant warts
- Good option for cosmetically sensitive areas
Immunotherapy Approaches:
Intralesional Immunotherapy: Injection of immune stimulants directly into warts can trigger a robust immune response against HPV infection.
Common Agents:
- Candida antigen injection
- Measles, mumps, rubella (MMR) vaccine
- Tuberculin purified protein derivative
- Interferon injections
Mechanism: These agents stimulate local and systemic immune responses, helping the body recognize and eliminate HPV-infected cells throughout the body.
Advantages:
- Can treat multiple warts with single injection
- Lower recurrence rates
- Useful for extensive or resistant cases
- Avoids tissue destruction and scarring
Chemical Treatments:
Trichloroacetic Acid (TCA): TCA in concentrations of 80-90% provides chemical cauterization of wart tissue.
Application Method:
- Precise application to avoid normal skin
- Immediate whitening indicates adequate treatment
- May require multiple applications
- Weekly treatments for several weeks
Cantharidin: Derived from blister beetles, cantharidin causes blistering that separates the wart from underlying tissue.
Treatment Process:
- Painless application in office
- Covered with adhesive bandage
- Blister forms within 24-48 hours
- Patient returns for debridement in 1-2 weeks
Surgical Interventions:
Electrosurgery and Curettage This combination approach uses electrical current to destroy tissue followed by surgical scraping to remove remaining infected material.
Procedure:
- Large, resistant warts
- When other treatments have failed
- Patient preference for definitive removal
- Multiple warts in localized area
- Local anesthesia administration
- Electrodesiccation to destroy tissue
- Curettage to remove loosened material
- May require multiple cycles
- Wound care and healing management
Indications:
Large, resistant warts
When other treatments have failed
Patient preference for definitive removal
Multiple warts in localized area
Considerations:
- Risk of scarring
- Requires local anesthesia
- Longer healing time
- Potential for recurrence at wound edges
Surgical Excision Complete surgical removal may be considered for very large warts or when malignancy is suspected.
Technique:
- Local anesthesia
- Full-thickness excision with clear margins
- Primary closure or healing by secondary intention
- Histopathological examination if indicated
Limitations:
- Highest scarring risk
- Requires surgical expertise
- Longer recovery period
- Reserved for special circumstances
Treatment Selection and Individualized Care
Age Considerations:
- Children may require less aggressive approaches
- Pain tolerance varies significantly by age
- Cosmetic concerns more important in adolescents and adults
- Immune system maturity affects treatment response
Location-Specific Approaches:
- Facial warts require cosmetically sensitive treatments
- Plantar warts need approaches that address depth and pressure
- Genital warts require specialized protocols and partner consideration
- Periungual warts near nails present unique challenges
Immune Status Assessment:
- Immunocompromised patients may need combination approaches
- Normal immune function predicts better treatment responses
- Previous treatment failures may indicate immune dysfunction
- Systemic immunotherapy may be beneficial in some cases
Treatment Algorithm:
First-Line Approaches:
- Topical salicylic acid for common warts in non-cosmetic areas
- Cryotherapy for most wart types in healthy individuals
- Observation in children with recent-onset warts
Second-Line Options:
- Combination topical and destructive therapies
- Alternative destructive methods (TCA, cantharidin)
- Immunotherapy for multiple or resistant warts
Third-Line Interventions:
- Laser therapy for resistant or cosmetically sensitive lesions
- Surgical approaches for large or persistent warts
- Combination immunotherapy and destructive treatments
Prevention Strategies and Patient Education
Primary Prevention:
- Regular hand washing with soap and water
- Avoiding direct contact with known warts
- Not sharing personal items like towels or razors
- Wearing shoes in public shower areas and pools
- Keeping feet dry and changing socks regularly
Skin Care Practices:
- Maintaining healthy skin barrier function
- Treating cuts and abrasions promptly
- Avoiding picking at existing warts or hangnails
- Using urea based moisturizers to prevent skin cracking
- Protecting hands during work activities
Environmental Precautions:
- Cleaning and disinfecting shared surfaces
- Using barrier protection in high-risk environments
- Avoiding walking barefoot in communal areas
- Choosing reputable facilities with good hygiene practices
Secondary Prevention:
- Regular self-examination of skin
- Prompt medical evaluation of suspicious lesions
- Early treatment to prevent spread
- Family member screening when indicated
Preventing Spread:
- Covering existing warts with bandages
- Avoiding activities that may spread infection
- Treating all warts simultaneously when possible
- Following proper wound care after treatment
Prognosis and Long-term Outcomes
Natural History
Spontaneous Resolution: Many warts, especially in children, resolve spontaneously within 2-3 years as the immune system develops specific responses to HPV. However, waiting for spontaneous resolution is not always advisable due to spread risk and patient discomfort.
Factors Affecting Spontaneous Resolution:
- Age (higher likelihood in children)
- Immune system status
- Wart type and location
- Duration of infection
- Number of lesions
Treatment Outcomes:
- Cryotherapy: 60-80% success rate
- Topical salicylic acid: 50-70% success rate
- Laser therapy: 70-90% success rate
- Immunotherapy: 60-80% success rate
- Surgical excision: 90-95% success rate
Recurrence Patterns:
- Local recurrence at treatment site: 10-30%
- Development of new warts elsewhere: Variable
- Factors affecting recurrence: Immune status, HPV type, treatment completeness
Long-term Complications:
- Scarring from aggressive treatment
- Pigmentation changes
- Functional impairment (especially plantar warts)
- Psychological impact and social concerns
Special Populations and Considerations
Immunocompromised Patients:
- More extensive wart development
- Resistance to standard treatments
- Higher recurrence rates
- Potential for atypical presentations
Modified Treatment Approaches:
- Combination therapies often necessary
- Immunotherapy may be particularly beneficial
- Longer treatment courses required
- Close monitoring for complications
Pediatric Considerations:
- Less aggressive approaches preferred
- Pain management crucial for compliance
- Parental education and involvement important
- Consider observation for recent-onset warts
Special Concerns:
- School attendance and activity restrictions
- Peer social interactions
- Long-term cosmetic outcomes
- Family transmission prevention
Conclusion:
Warts represent a common but complex dermatological condition requiring comprehensive understanding of viral pathogenesis, accurate diagnosis, and individualized treatment approaches. While numerous treatment options exist, success depends on proper patient selection, technique execution, and realistic expectation setting.
Key principles for successful wart management:
- Accurate diagnosis: Distinguish warts from other skin conditions through careful examination
- Individualized treatment: Consider patient age, location, immune status, and preferences
- Realistic expectations: Understand that multiple treatments may be necessary
- Prevention focus: Emphasize measures to prevent spread and recurrence
- Professional expertise: Seek appropriate medical care for optimal outcomes
- Patient education: Provide comprehensive information about condition and treatment options
Modern wart treatment offers numerous effective options that can provide complete resolution while minimizing complications and recurrence. At Derma & Dental Clinic, our experienced dermatologists utilize the latest evidence-based approaches to deliver safe, effective wart removal tailored to each patient’s individual needs.
Don’t let warts interfere with your daily activities or self-confidence. Contact us today for professional evaluation and personalized treatment plans that can help you achieve clear, healthy skin while preventing spread to family members and friends.
