Introduction
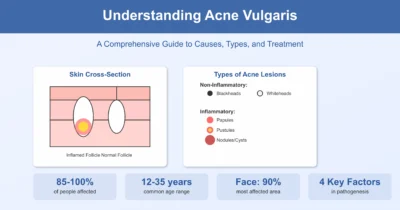
Acne vulgaris is one of the most common skin conditions worldwide, affecting 85-100% of people at some point in their lives. This chronic inflammatory disease of the pilosebaceous follicles can significantly impact quality of life, causing both physical and psychological distress. In this comprehensive guide, we’ll explore everything you need to know about acne, from its causes and symptoms to the latest treatment options.
What is Acne Vulgaris?
Acne vulgaris is a chronic inflammatory disease of the pilosebaceous follicle (hair follicle and its associated oil gland). It’s characterized by:
- Non-inflammatory lesions (comedones)
- Inflammatory lesions (red papules, pustules, nodules) in more severe forms
The condition primarily affects areas of skin with a dense population of sebaceous glands, including:
- Face (90% of cases)
- Back (60% of cases)
- Upper chest (15% of cases)
Understanding the Pathophysiology
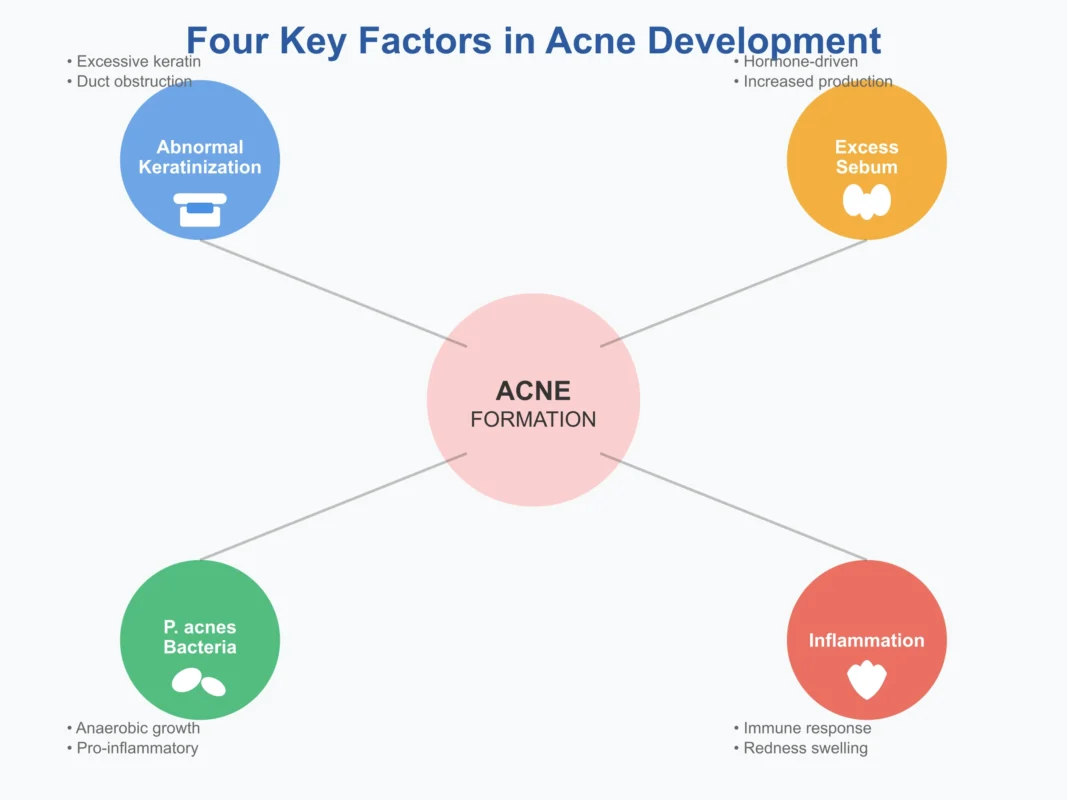
The development of acne is multifactorial, involving four key mechanisms:
1. Abnormal Ductal Hyperproliferation
This is the first recognized event in acne development. The exact cause isn’t fully understood, but contributing factors include:
- Androgen hormones
- Changes in lipid composition
- Pro-inflammatory mediators (especially IL-1)
2. Excessive Sebum Production
Various hormones and mediators regulate sebum production:
- Androgens
- Growth hormone
- Insulin-like growth factor
- End-organ hyper-responsiveness to hormones
3. Propionibacterium acnes (P. acnes)
This anaerobic organism promotes inflammation through:
- Production of pro-inflammatory mediators (IL-2, IL-8, TNF)
- Triggering hypersensitivity reactions
4. Inflammation
The inflammatory response is triggered by the combination of the above factors, leading to the characteristic red, swollen lesions of acne.
Clinical Features and Types of Acne Lesions
Non-Inflammatory Lesions
- Blackheads (Open Comedones)
- Sebum and keratin accumulate
- Appear as black papules
- The dark color is due to oxidation, not dirt
- Whiteheads (Closed Comedones)
- Appear as skin-colored papules
- Sebum and keratin accumulate beneath the skin surface
- Located at a distance from the follicular opening
Inflammatory Lesions
- Red papules – Small, raised, red bumps
- Pustules – Papules with visible pus
- Nodules – Large, painful, solid lesions deep within the skin
Healing Lesions
- Pigmented macules (post-inflammatory hyperpigmentation)
- Scarring (hypertrophic, keloids, or atrophic depressed scars)
Factors That Influence Acne
Genetic Factors
Family history plays a significant role in acne development and severity.
Medications
Certain medications can trigger or worsen acne:
- Steroids
- Lithium
- Antiepileptics
- Antituberculous drugs
- Iodides
Cosmetics and Personal Care
- Oily cosmetics and hair pomades can clog pores
- Occlusive products should be avoided
Hormonal Factors
- Pre-menstrual flare: About 70% of women experience acne flare 2-7 days before menstruation
- Endocrine disorders: PCOS, congenital adrenal hyperplasia, and other conditions with excess androgens
Environmental Factors
- Sweating: About 15% report acne flare with increased sweating
- Heat and humidity
- Occupational exposure: Catering industry, oil industry workers
Other Factors
- Excessive or vigorous washing
- Friction and pressure on the skin
- Manipulation of lesions (picking or squeezing)
Debunking Common Acne Myths
Let’s address some persistent misconceptions about acne:
- “You’ll grow out of it” – While acne often improves with age, it can persist into adulthood and requires proper treatment
- “Acne is caused by poor hygiene” – Acne is not caused by dirt; excessive washing can actually worsen it
- “Diet causes acne” – Scientific evidence linking diet to acne is limited; chocolate and greasy foods don’t directly cause acne
- “Vigorous washing helps” – Over-washing can irritate skin and worsen acne
- “Treatments don’t work” – Many effective treatments exist; patience and proper use are key
Psychological Impact of Acne
The psychological effects of acne shouldn’t be underestimated. Common impacts include:
- Stress and anxiety
- Embarrassment
- Lack of confidence
- Impaired social contact
- Anger and frustration
- In severe cases, suicidal ideation
Diagnosis and When to See a Doctor
While mild acne can often be managed with over-the-counter treatments, you should consult a dermatologist if:
- Acne is moderate to severe
- Over-the-counter treatments haven’t worked after 6-8 weeks
- You’re experiencing psychological distress
- There are signs of scarring
- You have signs of hormonal imbalance (irregular periods, excessive hair growth)
Laboratory Investigations
For certain patients, especially women with signs of hormonal imbalance, tests may include:
- Serum testosterone
- DHEA-S
- Pelvic ultrasound
Treatment Options
General Measures
Before starting specific treatments, consider these general recommendations:
- Avoid oil-based cosmetics
- Don’t manipulate or squeeze lesions
- Avoid topical steroids
- Skip fairness creams
- Avoid facials and massage during active breakouts
Topical Treatments
1. Retinoids
- How they work: Normalize follicular keratinization and have anti-inflammatory effects
- Common types: Tretinoin (0.05%), Adapalene, Tazarotene
- Usage: Apply at night (can cause photosensitivity)
- Side effects: Initial irritation, dryness, redness, temporary worsening
2. Benzoyl Peroxide
- How it works: Antimicrobial and anti-inflammatory
- Concentrations: 2.5%, 4%, 5%
- Usage: Start with lower concentrations for short periods (1-2 hours)
- Side effects: Irritation, bleaching of fabrics
3. Topical Antibiotics
- Common types: Clindamycin (1-2%), Erythromycin (2-4%)
- How they work: Suppress P. acnes and reduce inflammation
- Best practice: Usually combined with retinoids or benzoyl peroxide to prevent resistance
4. Other Topical Agents
- Azelaic acid (20%)
- Salicylic acid
- Sulfur preparations
Systemic Treatments
Oral Antibiotics
For moderate to severe acne:
- Tetracyclines: Doxycycline (100mg), Minocycline (100mg)
- Macrolides: Erythromycin (1g), Azithromycin (500mg alternate days)
- Duration: Often needed for 3-6 months or longer
- How they work: Inhibit P. acnes growth and have anti-inflammatory effects
Hormonal Therapy
For women with hormonal acne:
- Cyproterone acetate: Combined with ethinyl estradiol
- Spironolactone: 50-100mg daily
- How they work: Decrease sebum secretion by blocking androgen effects
Oral Isotretinoin
The most effective treatment for severe acne:
- Dose: 0.5-1 mg/kg body weight daily for 12-16 weeks
- Indications: Severe acne or moderate acne not responding to other treatments
- How it works:
- Inhibits sebum secretion
- Decreases P. acnes count
- Reduces inflammation
- Side effects:
- Dry skin, lips, and eyes
- Initial flare in some patients
- Teratogenicity (strict pregnancy prevention required)
- Monitoring: Pregnancy tests, CBC, liver function tests, lipid profile
Physical Treatments
For acne scarring and resistant lesions:
- Intralesional steroid injections
- Cryotherapy
- Laser therapy (Fractional CO2, Er:Glass for scarring)
- Dermabrasion
- Injectable fillers for depressed scars
Creating an Effective Treatment Plan
Successful acne treatment requires:
- Patience: Most treatments take 6-12 weeks to show significant improvement
- Consistency: Regular use as directed is crucial
- Combination therapy: Often multiple treatments work better together
- Maintenance: Continue treatment even after improvement to prevent recurrence
- Regular follow-ups: Adjust treatment based on response
Prevention and Long-term Management
While you can’t always prevent acne, you can minimize flare-ups:
- Use non-comedogenic skincare and cosmetics
- Cleanse gently twice daily
- Remove makeup before bed
- Manage stress
- Avoid picking or squeezing lesions
- Protect skin from excessive sun exposure
- Maintain a consistent skincare routine
The Importance of Professional Care
As emphasized by dermatology experts, acne is such a common problem that every medical professional should understand its basic concepts to manage patients effectively. Don’t hesitate to seek professional help, especially if:
- Your acne is affecting your quality of life
- Over-the-counter treatments aren’t working
- You’re developing scars
- You have signs of hormonal imbalance
Frequently Asked Questions (FAQs)
Q1: At what age does acne typically start and end?
A: Acne commonly affects people between 12-35 years of age, with peak incidence during teenage years. However, it can persist into adulthood, and some people develop adult-onset acne in their 20s, 30s, or even later.
Q2: Is acne contagious?
A: No, acne is not contagious. You cannot catch acne from someone else or spread it to others through touch or shared items.
Q3: Can makeup cause acne?
A: Yes, certain cosmetics can contribute to acne, especially oil-based or comedogenic products. Look for products labeled “non-comedogenic” or “oil-free” to minimize the risk of clogged pores.
Q4: How long does it take for acne treatments to work?
A: Most acne treatments require 6-12 weeks of consistent use before showing significant improvement. Some people may experience an initial worsening before improvement occurs, especially with retinoids.
Q5: Can diet affect acne?
A: While the PDF notes that scientific proof linking diet to acne is lacking, some recent studies suggest that high-glycemic foods and dairy products might worsen acne in some individuals. However, chocolate and greasy foods don’t directly cause acne as commonly believed.
Q6: Should I pop my pimples?
A: No, you should avoid manipulating or squeezing acne lesions. This can lead to increased inflammation, infection, scarring, and spreading of bacteria to other areas.
Q7: Can stress cause acne?
A: While stress doesn’t directly cause acne, it can worsen existing acne by triggering hormonal changes that increase oil production and inflammation.
Q8: Is it safe to use multiple acne treatments at once?
A: Combination therapy is often more effective, but it should be done under professional guidance. Using too many products simultaneously can irritate the skin and worsen acne.
Q9: What’s the difference between blackheads and whiteheads?
A: Both are types of comedones. Blackheads (open comedones) have an opening to the skin surface and appear dark due to oxidation. Whiteheads (closed comedones) are covered by skin and appear as flesh-colored bumps.
Q10: Can sun exposure help acne?
A: While sun exposure might temporarily dry out pimples, it can actually worsen acne in the long run by increasing inflammation and causing skin damage. Many acne medications also increase sun sensitivity.
Q11: When should I see a dermatologist for acne?
A: You should consult a dermatologist if:
- Your acne is moderate to severe
- Over-the-counter treatments haven’t worked after 6-8 weeks
- You’re developing scars
- Acne is affecting your self-esteem or daily life
- You have signs of hormonal imbalance
Q12: Can acne leave permanent scars?
A: Yes, especially inflammatory acne (nodules and cysts) can lead to permanent scarring. This is why early and appropriate treatment is important. Scars can be hypertrophic, keloids, or atrophic (depressed).
Q13: Is isotretinoin safe?
A: Isotretinoin is highly effective for severe acne but requires careful monitoring. Common side effects include dry skin and lips. It’s absolutely contraindicated in pregnancy due to severe birth defects. Regular blood tests are needed to monitor liver function and lipid levels.
Q14: Can birth control pills help with acne?
A: Yes, certain oral contraceptives containing cyproterone acetate and ethinyl estradiol can help reduce acne in women by decreasing androgen levels and sebum production.
Q15: Why does acne get worse before my period?
A: About 70% of women experience pre-menstrual acne flares 2-7 days before their period. This is due to hormonal fluctuations, increased duct hydration, and pro-inflammatory effects of estrogen and progesterone.
Q16: Can overwashing make acne worse?
A: Yes, excessive or vigorous washing can irritate the skin, strip natural oils, and trigger increased oil production, potentially worsening acne. Gentle cleansing twice daily is sufficient.
Q17: Are there any occupations that increase acne risk?
A: Yes, workers in the catering industry (due to heat and oil exposure) and oil industry workers have increased risk of acne due to environmental factors.
Q18: What’s the difference between acne and rosacea?
A: While both can cause facial redness and bumps, rosacea typically affects adults over 30, involves facial flushing, visible blood vessels, and doesn’t include comedones (blackheads/whiteheads) like acne does.
Q19: Can acne affect areas other than the face?
A: Yes, acne commonly affects the back (60% of cases) and chest (15% of cases), in addition to the face (90% of cases). Any area with a high concentration of sebaceous glands can be affected.
Q20: How can I prevent acne scars?
A: The best way to prevent scars is to:
- Treat acne early and effectively
- Never pick or squeeze pimples
- Use sun protection
- See a dermatologist for moderate to severe acne
- Consider professional treatments for existing scars
Conclusion
Acne vulgaris is more than just a cosmetic concern—it’s a medical condition that can significantly impact physical and emotional well-being. With proper understanding and treatment, most cases of acne can be effectively managed. Remember that successful treatment requires patience, consistency, and often a combination of approaches tailored to your specific type of acne and skin.
If you’re struggling with acne, don’t suffer in silence. Consult with a dermatologist to develop a personalized treatment plan. With today’s advanced treatments, clear skin is an achievable goal for most people with acne.
Remember: This information is for educational purposes. Always consult with a qualified healthcare provider for personalized medical advice and treatment.