Medical Conditions That Cause Dark Neck and Underarms: Complete Health Guide
Dark patches on your neck and underarms often signal underlying medical conditions that need attention. While acanthosis nigricans might seem like just a skin problem, it’s frequently your body’s way of indicating metabolic, hormonal, or other health issues requiring medical evaluation.
Understanding which medical conditions cause these dark patches helps you get proper treatment for both your skin and overall health. This comprehensive guide covers all major health conditions linked to acanthosis nigricans, their symptoms, and when to seek specialized care.
Diabetes and Insulin Resistance: The Primary Connection
Understanding Insulin Resistance
Insulin resistance is the most common medical condition causing acanthosis nigricans, affecting millions of people worldwide. When your cells become less responsive to insulin, your pancreas produces more insulin to maintain normal blood sugar levels. This excess insulin stimulates skin cell growth and pigment production, creating the characteristic dark, thick patches.
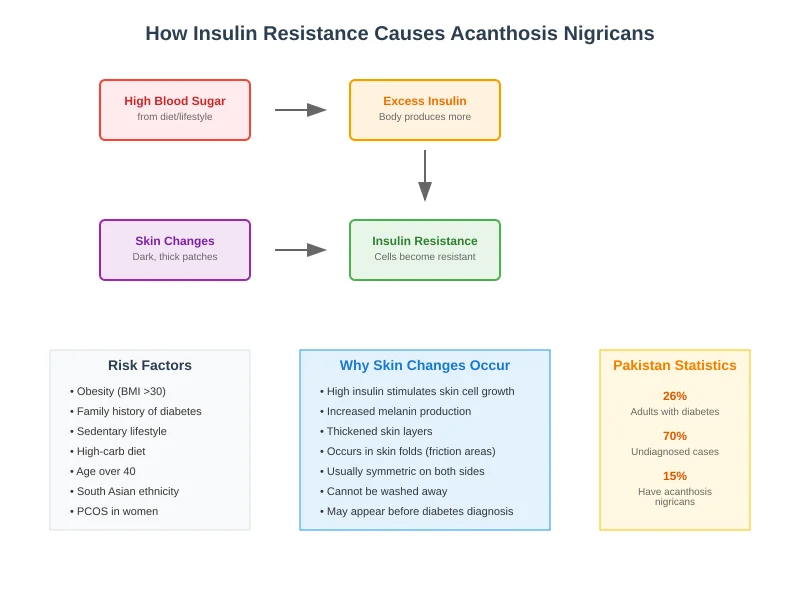
How insulin resistance develops:
- Cells gradually become less sensitive to insulin signals
- Pancreas compensates by producing more insulin
- High insulin levels activate growth factors in skin
- Skin cells multiply rapidly and produce excess pigment
- Dark, velvety patches appear in skin folds
Risk factors for insulin resistance:
- Central obesity (belly fat accumulation)
- Family history of diabetes
- Sedentary lifestyle with minimal physical activity
- Diet high in refined carbohydrates and processed foods
- Age over 40 years
- South Asian ethnicity (genetic predisposition)
- Previous gestational diabetes
- Sleep disorders including sleep apnea
Type 2 Diabetes Connection:
Acanthosis nigricans often appears years before type 2 diabetes is formally diagnosed, serving as an important early warning sign. Research shows that people with these dark patches have a significantly higher risk of developing diabetes within 5-10 years.
Diabetes symptoms to watch for:
- Excessive thirst (polydipsia)
- Frequent urination (polyuria)
- Unexplained fatigue
- Blurred vision
- Slow-healing wounds
- Frequent infections
- Unexplained weight loss or gain
Diagnostic tests for diabetes:
- Fasting blood glucose (>126 mg/dL indicates diabetes)
- Oral glucose tolerance test
- HbA1c levels (>6.5% suggests diabetes)
- Random blood glucose testing
Prediabetes and Early Intervention:
Prediabetes represents an intermediate stage where blood sugar levels are higher than normal but not yet diabetic. Many people with acanthosis nigricans have prediabetes, making early intervention crucial for preventing progression to full diabetes.
Prediabetes diagnostic criteria:
- Fasting glucose: 100-125 mg/dL
- HbA1c: 5.7-6.4%
- Oral glucose tolerance test: 140-199 mg/dL
Intervention strategies:
- Weight loss of 5-10% body weight
- Regular physical activity (150 minutes weekly)
- Dietary modifications focusing on low glycemic foods
- Regular monitoring of blood glucose levels
Hormonal Disorders and Endocrine Conditions
Polycystic Ovary Syndrome (PCOS):
PCOS affects 6-12% of reproductive-age women in Pakistan and is strongly associated with acanthosis nigricans due to underlying insulin resistance and hormonal imbalances.
PCOS symptoms accompanying acanthosis nigricans:
- Irregular or absent menstrual periods
- Excess hair growth on face and body (hirsutism)
- Male pattern baldness or hair thinning
- Weight gain, especially around the waist
- Difficulty losing weight
- Skin tags in addition to dark patches
- Severe acne that doesn’t respond to typical treatments
PCOS diagnostic criteria (need 2 out of 3):
- Irregular ovulation or anovulation
- Clinical or biochemical signs of hyperandrogenism
- Polycystic ovaries on ultrasound
Treatment approach for PCOS-related acanthosis nigricans:
- Metformin for insulin resistance
- Hormonal contraceptives for cycle regulation
- Anti-androgen medications (spironolactone)
- Weight management through diet and exercise
- Inositol supplementation for insulin sensitivity
Thyroid Disorders:
Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can contribute to acanthosis nigricans development through different mechanisms affecting metabolism and insulin sensitivity.
Hypothyroidism and acanthosis nigricans:
- Slowed metabolism leading to weight gain
- Reduced insulin sensitivity
- Changes in skin texture and pigmentation
- Fatigue and cold intolerance
- Constipation and depression
- Dry skin and hair loss
Hyperthyroidism considerations:
- Increased metabolic demand affecting insulin
- Rapid weight changes
- Heat intolerance and excessive sweating
- Anxiety and restlessness
- Rapid heartbeat
Thyroid function testing:
- TSH (Thyroid Stimulating Hormone)
- Free T4 and T3 levels
- Thyroid antibodies when indicated
- Regular monitoring during treatment
Cushing’s Syndrome:
Cushing’s syndrome results from prolonged exposure to high cortisol levels and can cause acanthosis nigricans along with other distinctive symptoms.
Cushing’s syndrome symptoms:
- Central obesity with fat accumulation around midsection
- Purple stretch marks (striae)
- Easy bruising and poor wound healing
- High blood pressure
- Muscle weakness
- Mood changes including depression
- Acanthosis nigricans in skin folds
Diagnostic approach:
- 24-hour urine cortisol collection
- Dexamethasone suppression test
- Late-night salivary cortisol
- Imaging studies when indicated
Growth Hormone Disorders:
Acromegaly, caused by excess growth hormone, can lead to acanthosis nigricans along with characteristic physical changes.
Acromegaly symptoms:
- Enlarged hands and feet
- Coarse facial features
- Joint pain and arthritis
- Sleep apnea
- Excessive sweating
- Skin tags and acanthosis nigricans
- Diabetes and insulin resistance
Obesity and Metabolic Syndrome
Obesity as a Primary Cause:
Obesity is one of the most common causes of acanthosis nigricans, particularly when fat accumulates around the abdomen (visceral obesity). The relationship between obesity and dark patches is primarily mediated through insulin resistance.
Obesity-related factors contributing to acanthosis nigricans:
- Visceral fat produces inflammatory substances
- Increased insulin resistance
- Hormonal imbalances including leptin resistance
- Mechanical friction in skin folds
- Chronic low-grade inflammation
Body mass index (BMI) considerations:
- Normal weight: BMI 18.5-24.9
- Overweight: BMI 25-29.9
- Obese: BMI 30 and above
- Morbidly obese: BMI 40 and above
Metabolic Syndrome:
Metabolic syndrome represents a cluster of conditions occurring together that increase diabetes and heart disease risk. Acanthosis nigricans often accompanies metabolic syndrome.
Metabolic syndrome criteria (need 3 out of 5):
- Waist circumference >40 inches (men) or >35 inches (women)
- Triglycerides ≥150 mg/dL
- HDL cholesterol <40 mg/dL (men) or <50 mg/dL (women)
- Blood pressure ≥130/85 mmHg
- Fasting glucose ≥100 mg/dL
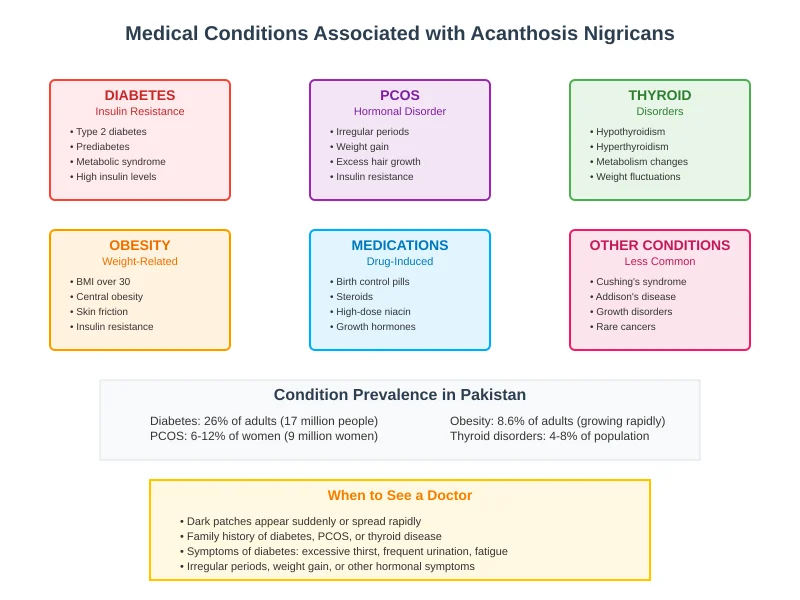
Medication-Induced Acanthosis Nigricans
Common Medications Causing Dark Patches:
Several medications can trigger or worsen acanthosis nigricans by affecting insulin sensitivity or hormonal balance.
High-risk medications:
- Corticosteroids: Prednisone, hydrocortisone, dexamethasone
- Hormonal contraceptives: Especially high-androgenic formulations
- Niacin (Nicotinic acid): High-dose formulations for cholesterol
- Protease inhibitors: Used in HIV treatment protocols
- Growth hormone preparations: Therapeutic and non-medical use
- Some antipsychotic medications: Particularly atypical antipsychotics
Mechanism of medication-induced acanthosis nigricans:
- Direct effects on insulin sensitivity
- Hormonal pathway disruption
- Weight gain as a side effect
- Inflammatory responses
Management strategies:
- Medication review with healthcare provider
- Dose adjustments when possible
- Alternative medication options
- Monitoring for improvement after discontinuation
Contraceptive and Hormone Therapy Considerations:
Hormonal medications, particularly those with androgenic activity, can trigger acanthosis nigricans in susceptible individuals.
Contraceptive options with lower risk:
- Low-androgenic progestins
- Lower estrogen formulations
- Non-hormonal contraceptive methods
- Regular monitoring when using hormonal methods
Familial Acanthosis Nigricans:
Some cases of acanthosis nigricans have a strong genetic component, appearing in multiple family members across generations.
Characteristics of hereditary acanthosis nigricans:
- Earlier onset (childhood or adolescence)
- Often more extensive distribution
- May occur without obvious metabolic abnormalities
- Strong family history pattern
- Associated with genetic syndromes
When to Seek Specialist Care
Endocrinology Referral Criteria:
Consider endocrinology consultation for:
- Confirmed or suspected diabetes/prediabetes
- PCOS diagnosis and management
- Thyroid disorders requiring specialized care
- Suspected Cushing’s syndrome or growth hormone disorders
- Complex hormonal abnormalities
Dermatology Consultation Indicators:
Dermatology referral appropriate for:
- Extensive or rapidly progressive skin changes
- Cosmetic concerns about appearance
- Professional treatment options (peels, lasers)
- Difficult-to-diagnose skin changes
- Concurrent skin conditions
Oncology Evaluation:
Urgent oncology referral for:
- Sudden-onset extensive acanthosis nigricans
- Associated unexplained weight loss
- Oral mucosal involvement
- Age >50 with new-onset disease
- Failure to respond to standard interventions
Diagnostic Approach and Testing:
Comprehensive evaluation should include:
- Complete medical history
- Physical examination including skin assessment
- Family history of diabetes and metabolic disorders
- Medication review
- Assessment of symptoms suggesting underlying conditions
Laboratory Testing Recommendations
Initial screening tests:
- Fasting glucose and insulin levels
- HbA1c for diabetes screening
- Lipid profile
- Thyroid function tests (TSH, Free T4)
- Complete blood count
- Comprehensive metabolic panel
Additional tests based on clinical suspicion:
- PCOS: Testosterone, DHEA-S, LH/FSH ratio
- Cushing’s syndrome: 24-hour urine cortisol, dexamethasone suppression
- Growth hormone disorders: IGF-1 levels
- Malignancy screening: Age-appropriate cancer screening
Imaging Studies:
Imaging may be indicated for:
- PCOS: Pelvic ultrasound for ovarian morphology
- Suspected malignancy: CT/MRI of chest, abdomen, pelvis
- Cushing’s syndrome: Pituitary or adrenal imaging
- Growth hormone disorders: Pituitary MRI
Treatment Approaches for Medical Conditions
Diabetes and Insulin Resistance Management:
Lifestyle interventions:
- Weight loss of 5-10% body weight
- Mediterranean-style diet emphasizing whole foods
- Regular physical activity (150 minutes moderate intensity weekly)
- Stress management and adequate sleep
Pharmacological interventions:
- Metformin as first-line therapy for insulin resistance
- Additional diabetes medications as needed
- Regular monitoring of HbA1c and glucose levels
- Lipid and blood pressure management
PCOS Treatment Strategies:
Hormonal management:
- Combined oral contraceptives for cycle regulation
- Metformin for insulin resistance and weight management
- Spironolactone for androgen excess
- Inositol supplementation for insulin sensitivity
Lifestyle modifications:
- Weight management through caloric restriction
- Low glycemic index diet
- Regular exercise including resistance training
- Stress reduction techniques
Thyroid Disorder Management
Hypothyroidism treatment:
- Levothyroxine replacement therapy
- Regular monitoring of TSH levels
- Dose adjustments based on symptoms and lab values
- Addressing concurrent nutritional deficiencies
Hyperthyroidism management:
- Antithyroid medications (methimazole, propylthiouracil)
- Radioactive iodine therapy when appropriate
- Beta-blockers for symptom control
- Regular monitoring of thyroid function
Prevention and Long-Term Management
Primary Prevention Strategies:
- Maintain healthy weight through balanced nutrition
- Regular physical activity from early age
- Annual screening for diabetes and metabolic disorders
- Genetic counseling for families with strong hereditary patterns
Secondary Prevention:
For those with existing conditions:
- Optimal management of underlying disorders
- Regular monitoring and medication compliance
- Lifestyle modifications to prevent progression
- Early intervention for complications
Long-Term Monitoring:
Follow-up recommendations:
- Regular dermatological assessment
- Diabetes screening every 1-3 years (based on risk)
- Hormonal monitoring for PCOS and thyroid disorders
- Cancer screening as age-appropriate
- Cardiovascular risk assessment
Conclusion:
Medical conditions causing acanthosis nigricans require comprehensive evaluation and management. While the skin changes themselves are often cosmetically concerning, addressing underlying health issues is crucial for overall well-being and often leads to improvement in skin appearance.
Early recognition and treatment of conditions like diabetes, PCOS, and thyroid disorders can prevent serious complications while improving quality of life. Regular medical monitoring and healthy lifestyle choices remain the foundation of successful long-term management.
For comprehensive evaluation of medical conditions associated with acanthosis nigricans, consult with experienced healthcare providers who can provide appropriate testing, diagnosis, and treatment recommendations tailored to your specific situation.
Medical Disclaimer: This information is for educational purposes only. Always consult qualified healthcare providers for diagnosis and treatment of medical conditions.